Snapshots of Dementia: I Bowed on My Knees
Tom directs an outdoor Christmas choir performance, c. 2014 How it’s going: — Tom asks for help much more often with the word games he plays on his iPad; sometimes he can’t fill in any of the missing letters or words on his own. — At bedtime, he sits on the side of the bed, staring into space, until I tell him it’s OK to lie down and go to sleep. — He occasionally tries to tell me about something that bothers or upsets him, but his sentences make no sense. The prediction his neurologist made last year was accurate: Tom’s decline has been more rapid this year than in the past. He’s had two major falls in the last three months, although neither caused severe injury. In short, life has become more challenging for him and for those of us who love him. But none of this either surprises or challenges God. My late friend and writing partner, Walker Moore, used to remind those in difficult situations, “The heavenly Father is not calling an emergency meeting over your life.” I know this still applies to my husband. Last Thursday, as we do twice a month, we traveled with the Joy Singers (senior adult choir) from our church to a local nursing home. We spoke with the residents for a few minutes before presenting our usual mini-concert of popular hymns and old-time Sunday school favorites. And then it happened. Our minister of music began the solo that ends most of our sessions, “I Bowed on My Knees and Cried Holy.” I stood with my fellow choir members, eyes closed for part of the time, as we listened and worshipped. But Tom was looking straight ahead. And as he did, he noticed tears rolling down the face of one of our fellow choir members—not an uncommon response to this song, which describes a Christ-follower’s first moments in heaven. Before long, he whispered to me, “I want to go over and sit with that lady” (whose name he doesn’t remember). Of course, I told him that was fine. He walked over to join her on the little couch where she and one of the residents sat. Before long, he wrapped his arms around her shoulders as tears poured down his face, his concern obvious to all. I don’t think he said anything, but he didn’t need to. The sense of awe this song brings us grew exponentially; we all sensed we were watching God at work. As the song finished, he gave our friend a final comforting hug and returned to my side. We and our fellow choir members spoke with a few more residents before leaving for lunch at a local restaurant. Our friend had a special reason for her tears. Only days before, she had received a concerning diagnosis of recurrent cancer. Although doctors had not yet outlined a specific plan, she knew she was facing surgery and months of treatment. Because Tom’s memory is so short, although I was praying for our friend, I had not yet told him of her situation. And apparently, I didn’t need to. The Spirit of God is more powerful than dementia or the apathy it often brings. Tom’s blank expression and lack of verbal response may often make him seem uncaring, but...
read moreSnapshots of Dementia: Pluses in the Minus
geralt on Pixabay Dementia steals. Dementia kills. Dementia destroys. Those of you familiar with Scripture will recognize that these are all tactics of the enemy of our souls. I have no doubt that Alzheimer’s and all dementia originates in his domain. But with or without familiarity with Scripture, you’ll recognize that I am a person of faith—a faith that has sustained me while Tom is living with dementia. As a result, I believe God can bring good for him, for me, and for others even in this present darkness. Dementia has indeed brought some positives into our lives. Many of these are small—but then again, small things are often the most essential. Here are a few ways the fact that Tom is LWD has added to rather than subtracted from our lives. Dementia has: • Moved me into a new position of strength. As I’ve written before, throughout our marriage, I too often stayed in the background, letting Tom take the lead even in areas where I was potentially more capable. Dementia has forced me to assume more responsibility, to do more and, more importantly, to be more than ever before. In this way, it has helped me grow into the person God knew I was all along. • Brought our family closer in fresh ways. I don’t think we “needed” dementia to help our relationships; we were already a loving, caring, imperfect family who enjoy spending time together. But without dementia, I doubt we would have moved as close to two of our daughters as we live now, much less had our son move in with us for a season. I doubt we would see our grandsons as regularly as we do or had the opportunity to attend so many ball games, school events, and birthday parties. We wouldn’t have heard first words or seen first smiles. We wouldn’t have had the opportunity to see our kids and their spouses step in when we had no choice but to call for help—both now and in times to come. • Moved us to the receiving end of ministry. We’ve given days and years to serving God, often through the church. For the first time in most of our forty-year-plus marriage, we now give much less than we receive. In the simple prayers Tom prays with me at morning and night, he almost always thanks God for our church. I know the gifts of relationships and kindness the many friends from our churches, past and present, bring our way lie behind his gratitude—and mine too. • Slowed us down. For our final years in Orlando, Tom and I were both working full time—and for me, that meant my first time of employment outside the home since our oldest daughter was an infant. I also kept some of my previous freelance work, which meant that between 2016-2018, I was working an average of sixty hours a week, added to Tom’s similar hours as a minister of music and pastoral care. Today, although I still work full time and sometimes more, I work from home, stopping multiple times a day to help him and make sure he’s safe. He doesn’t hesitate to ask me for help, and I always have an ear out for him and his activities. Because he gets tired easily, we...
read moreSnapshots of Dementia: Tom, Marti, and the Terrible, Horrible, No-Good, Very Bad Rehearsal
Tom, age eleven, plays his first nightclub job. Just as my brain is wired for words and language, Tom’s is wired for music. He has always been the guy who noticed the music in the store or restaurant that most of us hear only with our subconscious. In fact, if said music wasn’t to his liking, which was often, he was also the guy who would ask, maybe even insist, that the person in charge turn down the volume. He was the guy who could instantly create—and play—a trumpet descant for any hymn. He was the guy who wrote our wedding processional for five trumpets, two trombones, and a snare—and arrived at the church at 8 a.m. the day of our midmorning wedding to rehearse the musicians one final time (I believe some doughnut bribery may have occurred). And he was the guy who had to sit through all the credits to every movie so he could see who wrote the score and which musicians played which parts. Tom has spent much of his life making music. He has played the trumpet since he was nine years old. (I think most of our friends in Seneca can tell the story of him playing his first nightclub job at age eleven—they’ve all heard it a time or three.) He no doubt started singing at an even younger age. One summer in high school, he attended a music camp as a trumpet player and was picked for the select choir as well as the band. During seminary, he took time out to play his horn for two different Christian music groups, one of which was renowned contemporary Christian music group TRUTH. For the other group, he also served as keyboard player and music director. Only in college had he discovered what was probably obvious to his early music instructors: He has perfect pitch. Despite this obvious musical passion, he earned a Master of Divinity with full intentions to become a pastor-teacher, which he was for a number of years. But the pull to music was too strong. Ultimately, he shifted from being a senior pastor who could also do music to a worship pastor who could also preach. Now, he can no longer preach, and he doesn’t seem to mind. But music remains important to him. One gerontology nurse told us his musical aptitude would be one of the last things he would lose—both because the brain of the person LWD often retains music better than other abilities and because of how important music has been to him throughout his life. This should help explain why, despite my self-proclaimed lowering of expectations, I’ve struggled to let go of my expectations regarding Tom and music. I would tell myself and others. “He may remember his music when he doesn’t remember me.” I love singing with Tom in our choir and senior adult choir, and I have an adequate voice. But of the two of us, we both know he is the real musician. Today, after LWD for several years (we’ll never know just how long), he retains his perfect pitch, beautiful tenor voice, and ability to play the trumpet, although lack of practice has taken an obvious toll. But he is losing the ability to follow a musical score. ...
read moreSnapshots of Dementia: Great Expectations
Geralt on Pixabay Don’t have unrealistic expectations of your spouse. I had that advice drilled into me even before my marriage. I learned not to expect Tom, who had been raised in a far different family setting from mine, to do, say, or think things exactly as I did. I learned not to expect Tom, who was a pastor and spiritual leader, to be the perfect husband and father any more than I could be the perfect wife. And I learned that neither of us should expect the other to change. Instead, Tom and I learned, albeit slowly and sometimes painfully, to talk and pray through our differences. Sometimes he changed. Sometimes I changed. More often than not, we both did. Having an increasingly loose hold on expectations has helped me survive without too many scars before and since our living-with-dementia journey. I say “increasingly loose” because as Tom’s dementia changes him, I must change my expectations too. I wrote about how he stopped taking care of our lawn a few years before we knew he was LWD. Once I realized he was not going to take care of it (although I had no idea dementia was a factor), I stopped expecting him to do so. But when we packed up our Florida home, downsized, and moved to South Carolina in November nearly four years ago, it bothered me somewhat that Tom didn’t help at all. He didn’t sort a single item or pack a single box. In fact, his attempt to box up the theology books he sold to an online bookstore became an organizational disaster that brought me hours of extra work. That incident helped lower my expectations. I understood: Tom could no longer pack. And I didn’t want him to. At that time, since we didn’t have any sort of dementia diagnosis for Tom, I was still operating in a not-so-magical neverland, not knowing what he could and couldn’t do or what I should and shouldn’t expect. After he lost three jobs in a row, I decided he could no longer work. I no longer expected him to do so. After he had some near-misses with the car, our family decided he could no longer drive. We no longer expected him to do so. And after both of these changes and more, I decided to move closer to family—whether or not Tom’s doctors ever agreed he had a problem. I no longer expected him to have the wisdom to make such a big decision in a wise, caring way. All of these decisions shaped our expectations of Tom. But none of us had a real idea how much the expectations would continue to shift as we went along. Here are some of the ways even my recent expectations have changed: — I don’t expect Tom to remember anything I tell him. Sometimes I’m still caught off guard when he forgets something I’ve said only moments before, but I shift quickly into reality mode. One evening this week, I told him I was going out to the freezer to get something I needed for dinner. When I returned less than a minute later, he was making a peanut butter sandwich for his dinner (which I’ve never asked him to do), surprised that I planned to prepare anything. — I don’t...
read moreSnapshots of Dementia: How Firm Thy Friendship
by Andrew Pieper The silver sousaphone shone like a mirror in the Saturday afternoon sun as the band member high-stepped out of formation to dot the i with an exaggerated bow in the iconic Script Ohio, one of college football’s greatest traditions. The 100,000-plus fans in attendance roared their approval, and my dad smiled, enjoying once again the grand spectacle that is Ohio State football. Arriving in Ohio Friday afternoon, we drove an hour north of Columbus to visit the famous Ohio State Reformatory, which not only had served as a real prison until 1990 but also as the filming location for The Shawshank Redemption among other Hollywood movies. The chairlift hummed as it carried me—along with my dad in his wheelchair—up the side of the stairs. The wheelchair was a new addition to our travels. My dad is still able to walk with a walker, but he does so slowly and often with great pain. We decided to borrow a wheelchair for this trip, which made the whole experience much easier for both of us. Once inside, I purchased tickets for a guided tour. These tours are public and quite popular, often with up to forty people in attendance. But once our guide saw my dad in his wheelchair, he instructed the front desk to close the tour to make it easier for us to take the elevators up and down inside the prison. For the next ninety minutes, we had a private tour of every level, our guide sharing equal amounts of Shawshank history and that of the prison itself. After returning to Columbus and checking into our hotel, I made sure to connect my dad’s iPad to the Wi-Fi so he could play his online golf game. Regular routine has become an important part of his life, and the golf game is a big part of that routine. In fact, when I first asked him if he would like to go to another Buckeyes game, the first thing he asked was, “Will I be able to play my golf game?” Once he finished that day’s round, I drove him over to the Ohio State campus to watch the band rehearse. I could tell he was tired, but he seemed to enjoy the experience, tapping his hand in time with the beat. The following day, we arrived on campus three hours prior to kickoff. We were fortunate enough to grab one of the last parking spaces before the handicap lot was completely full. I wheeled him inside St. John Arena, where the band holds its skull session prior to every home game—a pep rally where the band plays a few songs, the football team is present, and the coach gives a speech before everyone heads to the stadium. The excitement built as, seated only a few dozen feet from the band and the team, we enjoyed the performance of several Ohio State classics, including “Hang on Sloopy,” with everyone, including my dad, joining to form the letters “O-H-I-O.” Rather than fighting our way through the tens of thousands of people walking toward the stadium as we had the previous year, we were able to board a handicap shuttle that dropped us right outside the gate. Once inside, we attempted to make our way to...
read moreSnapshots of Dementia: Have Dementia, Will Travel (Part 2)
Tom and Marti, Alaska 2023 We chose the trip together. We talked about it for months. We met with our friends to plan our off-ship excursions. But even the week we left, Tom didn’t remember what day we were going, what city we would fly into, or any of the other details of our Great Alaskan Adventure cruise. His dementia has progressed to the point that I can’t assume he remembers—or even understands—much at all. He still surprises me sometimes with what he does process well, but he surprises me much more often with what he doesn’t. This happened with the Steven Curtis Chapman part of our cruise: short sessions of Bible teaching, worship, reminiscing and even a Q&A with the Chapmans. We skipped a “Stump Stevie” night because of its late-night scheduling, but we attended all the other sessions. Tom at one of the SCC sessions For some foolish reason, I thought an artist who meant as much to him as SCC would somehow move him to engage. A nice idea, but that’s all it was. More accurately, it was magical thinking on my part. He didn’t seem unhappy, and he always said he was enjoying the trip—but it was hard to tell from his almost-standard expressionless face. One thing he did enjoy, however, was mealtime. This adventure had the standard cruise blessing (and curse): wonderful, plentiful food. We usually ate in a dining room with multiple buffet lines. The choices, of course, were too much for Tom. Sometimes he walked with me as I filled his plate other times, he sat with our friends while I got his food. He’s never been a foodie, but in the past, he would have especially enjoyed the various international options offered. His favorites on the cruise looked not-so-suspiciously like what he most enjoys at home: Breakfast omelets. Cheeseburgers (So. Many. Cheeseburgers.) Macaroni and cheese. Cookies. And as a special bonus blessing, ice cream. Although I did get him to venture away from cheeseburgers sometimes, he seemed happiest with his familiar favorites. Sure, it was way more red meat than he would have had at home, but the cruise only lasted a week. And a fortieth anniversary only comes around once. Tom had some physical challenges on our trip as well. He uses a walker because of a back problem. He can’t have the needed surgery because general anesthesia could exacerbate his cognitive decline. The relatively short trips around the ship required far more walking than he normally does in one day, so his back was already tired. Excursion days—although we chose those with only minimal walking—exhausted him. We almost always had a long walk as we left the ship, so the “few steps” promised for the excursion became many more. If I had known this in advance, I would have brought a wheelchair rather than a walker. The day we went on the White Pass & Yukon Railway resulted in terrible physical pain for Tom. We met in the same large room that hosted the SCC concerts, so that part seemed easy. But after we arrived, the people in charge hurried us off the ship to catch trams to the waiting buses that would take us to the train. Avoiding the normal long walk from ship to bus might have been a good thing. What wasn’t good?...
read moreSnapshots of Dementia: Have Dementia, Will Travel
Happy anniversary, baby!” I told Tom as we woke up on board the first day of our Great Alaskan Adventure Cruise. He didn’t respond. “I’m saying that because we’re on this trip to celebrate our fortieth anniversary. And I’m going to tell you that every day of this trip!” He smiled. But beyond that, I never received a response any of the mornings when I wished him a happy anniversary. One day, however, he surprised me. He proudly told our friend Hardy at lunch, “Today is a special day. It’s our anniversary!” Not quite. But I knew he had listened to my greeting after all. And this time, I was the one who smiled. Just as they do at home, small incidents like these embedded themselves in our trip to Alaska. When someone is living with dementia, the disease is the ever-present but unwelcome guest. Because we traveled across the country, dementia did too. Because we went on a cruise, dementia came along. And when we came home, dementia joined us—because it never left. As I wrote a few weeks ago, the presence of our friends Hardy and Barbara made the entire trip much more doable—and much less stressful—for Tom and me. Think about just one scenario: restroom use when someone is LWD. I typically walk Tom up to the door of the restroom and wait outside, but it still scares me because his memory is so short. What if he forgets that I’m waiting for him? Or doesn’t remember which way to turn so he can exit? Family restrooms are helpful not only for those with small children, but because they are both rare and busy, Hardy’s assistance proved invaluable, beginning in the airport before we left. Before the trip, I learned something that also helped us: The sunflower is a globally recognized symbol for those with hidden disabilities, and many airports—including the two we would visit—train their employees in the Sunflower Program. Before our trip, I bought Tom this lanyard; he wore it to hold his state-issued ID. Because no one ever mentioned the sunflower, I don’t know if its presence helped us or not. But it made me feel much safer to know he was wearing a symbol that airport workers would recognize, especially if we somehow got separated. (The only time that became an issue was on the way home, when workers took him one way to get through security and forced me into another line, then delayed me while they searched one of our bags. I don’t mind saying that that was a scary few minutes.) I brought along two more items that made the trip much more pleasant for Tom: his iPad and his weighted blanket. I knew he would need the iPad to play his daily word games and online golf game; preserving at least this much of his normal routine can help a lot with the agitation that often accompanies travel for people LWD. Although I had purchased Wi-Fi ahead of time so he could keep playing his games during the cruise, the signal was generally not strong enough to allow him to play the golf game. He accepted this change better than I feared, partly because we were so busy with other activities. He could still...
read moreSnapshots of Dementia: The Great Alaskan Adventure, Part 2
(L-R) Sheryl, Marti, Tom, and David in our first meeting on the ship Our Great Alaskan Adventure taught us—in more ways than one—how thankful we are that “I’ve Got a Friend Like You.” We knew we’d be traveling with Barbara and Hardy (see Part 1 of “The Great Alaskan Adventure” if you missed it.) But we didn’t know that we’d also be traveling with friends we have known for more than thirty years. David and Sheryl Neal were members of the second church Tom pastored, located in Southern California. Their three children are close to the same ages as our oldest three children, and when our fourth child and third daughter decided to come more than five weeks early, the Neals got the early-morning phone call and child-sitting duties. David and Sheryl have remained our friends through the many years and moves. Whenever we went back to the area, we made sure to visit them, even staying in their home for a few days on our last trip there. Sheryl and I have stayed in touch via emails, phone calls, and texts about joys, sorrows, and prayer needs along the way. The day before we left for Seattle, where we would embark on our cruise, one of our foster grandchildren (who happens to live with that fourth child of ours) required emergency surgery. Of course, I texted Sheryl to pray. In the process, I mentioned that I was out running final errands for our cruise, which apparently I’d forgotten to tell her about. “Wait, we leave for an Alaskan cruise Friday,” she texted back. I didn’t even consider the possibility that it might be the same cruise. I knew other couples who had gone to Alaska this summer, and I also knew multiple cruise lines cover that route. Still, Sheryl asked me to share the details (see text exchange below). I didn’t actually faint, but I’m sure I came close to it. And I’m thankful we have the photos to prove that we ended up on the same ship. For them, this was a Celiac Cruise; Sheryl has navigated her way through celiac disease for some time, and the wonderful invention of unique cruise, complete with a private dining room and chef, has made travel possible for her once again. Will Tom remember us? the Neals wondered ahead of time. When Sheryl mentioned this to me, I assured her he would. He might not remember the names of the couples he sees in Sunday school every week, but he would remember these dear and longtime friends. I had no doubt. We all boarded the ship Saturday but couldn’t connect until Sunday. I had told Tom before we left that David and Sheryl would be on the ship, but that day, he didn’t realize we would round a corner and see them coming toward us. His eyes widened in shock. “I HAVE MISSED YOU SOOOO MUCH!” he told David as he wrapped him in a giant hug. We sat down and talked, and talked, and talked—at least David, Sheryl, and I did. Tom mostly sat and listened, happy to enjoy our time together in his own way. We had excursions at opposite times the next day, so, since shared meals weren’t an option, we decided another meeting would have to wait till...
read moreSnapshots of Dementia: The Great Alaskan Adventure, Part 1
(L-R) Mary Beth Chapman, Hardy Lee, Barbara Winkler, Tom, Marti, Steven Curtis Chapman Our family loves music. Not just because Tom worked as a professional musician and worship pastor before he was living with dementia, although that has a lot to do with it. We can all name songs that meant a lot to us at various points in our family’s life—many of them from the contemporary Christian genre. One of the artists who has had a great impact on our lives is Steven Curtis Chapman, who also happens to be the most-awarded Christian music artist of all time. Tom and I have laughed, cried, and sung along with his music for much of our marriage; he released his first album the year our first two daughters were born, and his “Cinderella” played at the daddy-daughter dance for a family wedding. Just as his songs have accompanied our lives, they also became the soundtrack for our trip. The second listed below, which also features SCC, is by his longtime friend Geoff Moore and is also a family favorite. Enjoy and excuse the hairstyles! ‘The Great Adventure’ Because I knew Tom and I would celebrate our fortieth anniversary this summer, when I saw a magazine ad last fall for a week-long “Great Alaskan Adventure” cruise with Stephen Curtis and Mary Beth Chapman and friends (including Geoff Moore), an idea sparked. Could we? “I’ve always wanted to go to Alaska!” Tom said when I showed him the ad. The fact that he remembered the idea and mentioned it several days in a row also spurred me onward. Had I seen the ad a month or two earlier, I might not have had the courage to do anything about it. But our son’s own great adventure in taking his dad to an Ohio State football game last fall, along with our four daughters’ enthusiastic approval of the idea, gave me the courage to plan the trip. Whale watching in Juneau, Alaska For one full week in July, we had the incredible gifts of a mini-Christian conference with teaching from Scotty Smith, founding pastor of Christ Church, Franklin, Tennessee, and music from SCC and family/friends; the amenities of a luxury cruise ship; and the raw beauty of Alaska—including whale watching, a narrow-gauge railway ride up the White Pass and Yukon Route from Skagway, and gorgeous views of the Endicott Arm and Dawes Glacier—plus a guided bus tour of beautiful Victoria, British Columbia, complete with (for all my Canadian friends) a visit to Timmie’s! But wait. There’s more. ‘I’ve Got a Friend Like You’ We experienced many blessings during the trip, but the greatest came because of two sets of friends. One is a couple we’ve only known for a short time—in fact, they’ve only been a couple for a short time. Hardy Lee and Barbara Winkler, fellow members of our church, choir, and senior adult choir, were married this past December. Both were caregivers for their first spouses, now in heaven. When Tom learned of their upcoming nuptials, he offered to sing for their wedding. Not every couple wants a person LWD to take that role, but these two love Tom even more than they love music. I told them it might go well, or it might go just the opposite. “It’ll be fine,” Hardy assured me. And it...
read moreSnapshots of Dementia: What You Don’t See
(Unsplash) Marriage to someone who is living with dementia has taught me lots of things, many of which I’ve shared on this forum. I’ve learned about the disease, about the changing needs of people LWD, and about myself. I’ve also learned that, all along the way, there’s a lot those not in this situation don’t see—even when they spend time with someone LWD. This is true not because anyone is trying to hide or have secrets but simply because what we observe in a few minutes—or even a few hours—of anyone else’s life, LWD or otherwise, never gives us the whole picture. Even my snapshots of dementia, as transparent as I seek to be, are just that: snapshots, small glimpses, and usually from my own perspective. Although I’ve tried to give Tom’s perspective a time or two, that’s getting more and more difficult to share. Here, then, are some glimpses of what you do and don’t see (or would and wouldn’t see, if it were possible) when you see Tom and me: WHAT YOU DO SEE: Tom and Marti arriving at church, medical appointment, or another scheduled outing. WHAT YOU DON’T: The time it takes to get ready to leave. This includes last-minute bathroom trips or changes of clothes if he has spilled something along with finding sunglasses, reading glasses, sweater, and other necessary but often-misplaced items as well as (often) going back to close whichever door he exits and forgets to close. WHAT YOU DO SEE: Tom smiling and nodding, enjoying others’ company. WHAT YOU DON’T: Tom recalling fewer names and participating less and less in discussions because he can’t come up with quick responses. WHAT YOU DO SEE: Tom eating an unusually heavy meal, often with dessert. WHAT YOU DON’T: Tom’s lack of appetite control; he can eat a huge amount or very little without realizing what he’s doing or feeling either hungry or full. WHAT YOU DO SEE: Tom adding excessive amounts of salt, pepper, or both to his food. WHAT YOU DON’T: Tom’s dementia has stolen his sense of smell, which has diminished his sense of taste. As his dementia worsens, this seems to be worsening too. WHAT YOU DO SEE: Tom wearing a sweater, long sleeves, and long pants even when temperatures are in the eighties or nineties. WHAT YOU DON’T: Tom’s brain doesn’t process temperature well, and he is often cold. We keep a blanket in the car and a cardigan in the pouch on his walker to try to combat this problem. WHAT YOU DO SEE: Tom following behind me with his walker. WHAT YOU DON’T: Him becoming nervous and unsure where to go when I’m not in front of him. I used to stay behind to keep an eye on him, but now, that upsets him, so I either walk beside (when we have room) or directly in front of him and turn around often to check on him. WHAT YOU DO SEE: Beautiful photos of Tom smiling with our family, especially our grandchildren. WHAT YOU DON’T: The many times where he stares blankly into space or hyperfocuses on his iPad, ignoring everyone around him. WHAT YOU DO SEE: Tom continuing to sing in the adult and senior adult choirs. WHAT YOU DON’T: Him landing on the wrong page in his...
read moreSnapshots of Dementia: Living His Best Life
Tom with Lincoln and Lando, Father’s Day, 2023 When I made the decision to sell our home in the Orlando area and move to South Carolina to be near family, I often told people I hoped to “give Tom his best life.” At the time, I had little idea what that meant. So how do we give Tom his best life even while his brain continues to change? I’m still figuring it out. But here are some of the things that seem to help, despite many mistakes along the way. — ROUTINE: I’ve mentioned before how Tom can easily become agitated if too much of his routine changes. He likes to go out and enjoys being with friends and family, but he likes being home even more. We haven’t done much traveling since his diagnosis, but I’ve learned that trips go much better if I can keep mealtime, bedtime, and time for playing games on his iPad as close as possible to what we do at home. — FAMILY TIME: We spend most Friday nights with our oldest daughter and her family, who live nearby. Tom looks forward to this routine and especially to time with our two young grandsons. He also enjoys holidays, birthdays, and other family events. Earlier this spring, our youngest daughter blessed us with two week-long visits. And although our son hasn’t been here as much as he anticipated, every time he returns, Tom gives him a big hug and says how much he missed him. Relationships have always mattered to Tom, but while LWD, family seems to matter even more. — SOCIAL/SPIRITUAL: Attending church and singing in the choir and senior choir are becoming more challenging for Tom, but he still enjoys both. We stay active at church because it’s long been our priority and also because it’s a safe and healthy place for Tom. Friends there have consistently shown their concern for both of us, helping me get him safely from one place to another and making sure he’s not left out or left behind. I have long believed that those with cognitive challenges can still have a strong connection to God, and this holds true for Tom today. — DIET: I wrote here about some ways caregivers can stay healthy, and those choices have had an impact on Tom. I don’t experiment with new dishes too often; with his love for routine, familiar foods and longtime favorites make him happy. And although (with his doctor’s permission) I still ensure he has regular Wendy’s Frostys and other treats, I have shifted his diet to include more fruits, vegetables, and whole grains. Living his best life means staying as healthy as possible while his brain continues to change. — MEDICAL PROFESSIONALS: I can’t overemphasize the importance of a great health care team. Tom has developed other health issues alongside his dementia, so he sees some specialists in addition to his neurology team at the Emory Brain Clinic. The key piece, however, has been not the great neurological care but an excellent primary care physician. Our doctor has great insight into Tom’s dementia and shows concern for him as a person, not just a diagnosis. She also sees him once every three months, an extra reassurance for both of us. — COMMUNICATION: As Tom’s...
read moreSnapshots of Dementia: Life Is Hard
(Hans Peter Gauster, Unsplash) Life is hard, and it might not get easier.” Every one of our children knows this phrase well. While growing up, they often heard it from their dad (and eventually from each other as well as from me). It entered our lives as a line in an Amy Grant song, “We Believe in God.” Tom is living this reality now. Life with dementia is increasingly hard, especially in this year that has seen a steeper decline in his cognition and abilities. “What’s the hardest thing about living with dementia?” I asked him this morning. He had just misplaced his coffee mug and needed my help to find it, so although he hesitated, he had an answer. “Well, two things. First, I can’t remember where stuff is.” “Second …,” He gave one of his now-characteristic lengthy pauses, and after a couple of minutes had passed, I reminded him of the question. “Well, second (another long pause) … I’m sorry, I don’t remember.” “That’s OK, baby, I was just wondering what you thought. Is there something that really bothers you about having dementia?” “(Long pause) “If I think of something later, I’ll let you know.” I recently had to fill out a survey for an upcoming doctor’s appointment Tom has with the Brain Clinic at Emory University. It had to do with activities of daily living, a term health care professionals used to describe an individual’s daily self-care activities. I’ve filled out this survey before (Tom hasn’t been able to answer any medical questions on his own since 2018), but this time, I noticed that in more categories than ever before, I answered either “does not perform” or “cannot perform without help.” The ADL questions referred to such activities as fixing meals, driving a car, and keeping track of medication. Tom can’t do any of those activities, and for most of the remaining ones on the list, he requires a lot of assistance. What the questionnaire doesn’t reveal is how much assistance he needs. Although pet care wasn’t on the list, he needs more and more help in caring for his beloved box turtles. Last year, he could go out to our backyard pen and feed them on his own. This year, I go with him. He might forget that he’s not supposed to climb into the pen, which poses a fall risk. He might forget why he’s out there, and I remind him to give the turtles their food, which I’ve helped prepare. And of course without my reminders, he would forget that he needed to feed the turtles at all. Other ways his life has become harder as his brain change becomes more marked include: —Increased spills. Tom’s fine motor skills are deteriorating. He can still feed himself with normal utensils, but I usually give him a soup spoon rather than a tablespoon because it’s easier to use. At least once a week, he spills his travel mug of coffee on the floor or table, either because he forgets to put on the lid or because he can’t control the tremors in his hands as he lifts the mug. I now check his clothing before we go anywhere; although I haven’t moved to the step of having him wear a towel or bib, his shirts and...
read moreSnapshots of Dementia: Meet Me in the Middle
I knew it would happen. I just didn’t know it would be so soon. I knew the day would come when our oldest grandson, who is now five and a half, would show more responsibility, be more careful, and have more understanding than my husband, who is living with dementia. I knew the day would come when our grandson’s brain, which is constantly growing, would work better and faster than my husband’s, which is constantly shrinking. I knew the day would come when the two would—in terms of cognitive ability—meet in the middle, one continuing to advance, the other continuing to decline. I knew it would happen. I just didn’t know it would hurt so much. I didn’t come to this realization in an instant, of course. In reaching this conclusion, I am probably several months behind. One of the places Tom and Lincoln both love is Chick-fil-A, Tom for the food and Lincoln for the play area (not to mention the ice cream). Over this school year, we have often picked Lincoln up on a Friday and taken him either to our house or this favorite spot for dinner and play time. When we visit our local Chick-fil-A, we have to walk across the drive-thru lane to enter the restaurant. I used to hold our grandson’s hand when we did this to make sure he stayed safe. But for the past several months, I’ve asked Lincoln to keep Grandpa safe. He walks beside Tom, holding his hand or his walker; looks both ways when we have to cross the drive-thru lane; and opens the door so Tom and I can go through first. In the past, I loved our trips to Chick-fil-A because it was one of the few places where Tom would engage with Lincoln. He would stay in the play area with him, hiding from him as he came down the slide, then jumping out to “scare” him. Even while LWD, he did his best to make sure Lincoln stayed safe. These days, I choose a table close to the play area because Tom rarely wants to go inside with Lincoln. I can monitor our busy boy from the table or, if I’m in the play area with him, keep an eye on Tom, who is usually sitting at the table, eating or staring into space. We can still do the same activity; it’s just different now. We can still enjoy our time together; it’s just different now. Tom’s still himself; he’s just different now. As time has gone on and his brain change has continued, I’ve made some necessary adjustments. Some of these have been big ones: Managing all our money. Becoming the sole breadwinner. Asking him to stop driving. But many have been smaller: Organizing his medication and making sure he takes it. Staying nearby whenever we go anywhere. Helping him more often with the word games he plays on his iPad because he can rarely o them alone. Not long ago, we tried another favorite activity with Lincoln: a visit to a local miniature golf course. We hadn’t done this for some time, so I saw big changes in both the big and the little boy. Lincoln was still enthusiastic—and sometimes impatient—in his play. But he was also much better at listening and following my instructions. ...
read moreSnapshots of Dementia: For Such a Time as This
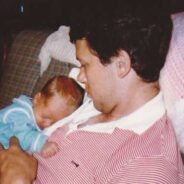
by Andrew Pieper Tom with baby Andrew, 1991 “OK, love you too, bye,” I said—my standard farewell on my weekly video calls with my mom and dad. Yet the call had felt anything but standard to me. The outside observer probably wouldn’t have noticed, yet there were subtle signs that left me with a sinking feeling. We had talked about many standard topics and events: church, work, happenings around town, but today I had to refresh my dad’s memory on multiple subjects, things we had talked about only a few days ago. Dad “knew” everything we talked about in great detail, yet he had no idea about any of them. This conversation lingered in my mind over the next week. I kept thinking of my dad, sitting there in his recliner, happy and content. Yet to me, who knew him as the witty, loud man who would often throw the childhood me up in the air to questionable heights of safety before gracefully catching me, he had become someone else entirely. Over the next several days, after a lot of thinking and praying about what I should do, I decided the best thing would be to pack my bags, leave Texas, where I had been living for a few months, and go to be with my parents for a while. Being the only boy among four sisters, my dad and I have always had a special relationship, but it’s changing now—and will continue to do so. Neither of my parents was ever “handyman inclined,” so whenever I came for visits, I assisted them with such tasks as replacing lights, pressure washing, and landscaping. By living with them, I could help alleviate some of the day-to-day tasks from my mom, who currently is wearing multiple hats, working full time while taking care of my dad, the house, and the yard. How long would this last? For the next six months? Six years? I have no clue on the timeline, but one thing that I strive to keep at the forefront of my thoughts is to have a heartbeat of obedience to God’s calling. I don’t want to have any preconceived “noes” in my mind for where God might call me or what He might call me to do. Just like that, I began the process of closing my storage unit and packing things up. Within two weeks I was ready to go; my van and trailer and I made the drive to South Carolina. It is only my second week since relocating here, and already God has given me multiple signs that this is the right move for this season of my life. First, my mom got sick with COVID this past week, so instead of primarily being concerned with the health and well-being of one parent, it has now been two. Thankfully, both my dad and I have tested negative, and while my mom’s energy has been wiped, she seems to be recovering now since taking some medication. The other day I was working on my motorcycle in the driveway, and my dad came out of the house, leaning on his walker. I looked up from my bike to see what he needed. “I was just wondering where you were,” he said, then turned and made his way...
read moreSnapshots of Dementia: That’s Just the Way It Is?
(Terri Cnuddle from Pixabay) It seemed easy enough. Some friends from our time in Charleston were visiting our small town and wanted to stop by for a brief visit. Trying to keep things simple, they planned to eat lunch before they came; we’d use our time together to talk and catch up. This visit was simple—much too simple when it came to Tom. For the most part, all he did was sit and listen to our conversation. Years ago, the woman and I had been part of the same homeschool group, and we eagerly discussed everything from where our children were living to the health of our mothers, now both widowed and in their 90s. My friend’s husband contributed here and there, but mine was almost completely silent. The only time he spoke was when I encouraged his agreement about one point or another as I continued my non-stop discussion. “You notice he’s hardly saying anything,” I mentioned to our friends when Tom stepped out of the room. They nodded. Before long, Tom was back, and we finished our visit much the same as we started it—the three of us doing most of the talking and Tom an almost-silent observer. Only after they left did I realize what I’d done—or what I hadn’t. In my eagerness to visit with my friends, I’d left Tom hanging in the breeze of our conversation. I’d acted as though I didn’t know how to interact with someone who is living with dementia. And worse, I’d behaved as though it didn’t matter. “That’s just the way it is,” I’d implied. Yes, that’s just the way it is—if I’m selfish. That’s just the way it is—if I’m not intentional. That’s just the way it is—if I don’t listen to the Holy Spirit about how to bless my husband. That’s just the way it is—if we don’t treat people LWD with the respect they deserve. Only a few days later, I invited another friend over for dinner. His wife was out of the country, and I thought he might enjoy some company and home-cooked food. As I prepared the meal, I realized that—both because of his love for Tom and his own prior caregiving experience—our friend would make a great co-laborer. Together, we could give Tom a different experience than I had with our previous guests, but it would require intentionality on both our parts. When our friend rang the doorbell, I made sure I answered. This is often what happens anyway because Tom tends to stay in his recliner, most often playing on his iPad. Our friend and I had a quick porch chat before entering the house. I told him about the recent visit and how Tom had largely remained silent. “This time, I’m going to try not to say too much,” I told him. “And I need you to think of things to ask him about. I’ll jump in sometimes, but I’m going to try to let him do most of the talking.” “I’m looking forward to it!” our friend said. We had a plan. Now, it was time to apply it. Although Tom loves and appreciates this friend, he barely looked up as I brought our friend into the family room. “I need to go finish up supper,” I told...
read moreSnapshots of Dementia: I Get That a Lot (and Why I Shouldn’t)
(TC Perch on Pixabay) You’re so patient.” “I don’t know how you do it.” “You’re an example for others.” I get that a lot. And to be honest, I shouldn’t. I understand why. In sharing snapshots of our life while living with dementia, I do my best to be as transparent as I can. But I know there are things I miss. And I also understand that my perspective is not the only one. When I teach on writing memoir, I encourage people to tell their own story, even if it’s not the way someone else remembers it. That’s what I seek to do here. So even though my story of LWD is not the same as someone else’s, it is my story—and thus our story, the best I can tell it, for both Tom and me. But I want to apologize for the times—past, present, and future—I may make myself sound better than I am. Because here’s the real truth: I am so not. Not patient. Not kind. Not good. Not any kind of example for anyone. Left to my own devices, I am just the opposite: impatient, prideful, selfish, self-centered, easily irritated, controlling, and so much more. In fact, I’m probably less likely than most people to be a good caregiver for someone who is LWD. But here’s the thing: The truths we celebrate this Easter weekend matter. And they changed my life. I grew up with two wonderful parents who faithfully took me to church. The sermons I heard and lessons I learned shaped my standards and values. But until my junior year in college, they reached no further than my intellect. If you had asked me back then, I could have told you that yes, Jesus died on the cross. I would have said that yes, God raised Him from the dead. And I would have also said that I might go to heaven someday, that I tried to do good things to gain that privilege. You see, I grew up trying to do lots of “good things” so I would avoid getting into trouble. That’s not a bad way to start out, but it’s not a great place to stay. And it didn’t give me a great picture of the God I know today. You see, that God created me to love and serve Him, to honor Him with my life. He knew I could never do that on my own. Remember? Left to my own devices, I am impatient, prideful, selfish, self-centered, easily irritated, controlling, and so much more. Until my college years, I didn’t understand that I could never be good enough for God; I needed Him to be good for me. His death on the cross was not a symbolic act but a personal one. He took the punishment I deserved. He died the death I earned. When I placed my faith in Christ, I not only received the promise that I will live with Him in heaven someday, but so much more: the unmerited ability to live a life I could never live without Him. The undeserved power to do that which I could never do on my own. So when someone tells me “You’re amazing,” or “I could never do what you do,” I want to tell them the truth:...
read moreSnapshots of Dementia: If You See Something, Say Something
(Israel Palacio on Unsplash) He’s quirky.” Anyone who’s known Tom through the years will agree that I wasn’t wrong when I described him this way to a group not long after we had come to the final church he served as minister of music. He’s a musician; I’m a writer—we pretty much understood that quirkiness was part of the package when we married each other. But now, I wonder just where his quirkiness stopped and the dementia behaviors began. And I don’t suppose I’ll ever know. I missed many of the early signs that Tom was living with dementia—partly because his neurologist and others kept telling me he was fine. But because I didn’t know about the behavioral issues dementia can cause, I am writing about them now so perhaps someone else won’t have to wait as long for a diagnosis as we did. Not everyone LWD exhibits these same behaviors, and not everyone LWD has as many behavioral issues as those with a variant that affects the frontal lobe. But in addition to those I noted last week, here are some more of the atypical behaviors we saw in Tom even before he received his dementia diagnosis: — IMPULSIVE/RECKLESS ACTIONS: I have written about how he was blackmailed via social media and later gave away thousands of dollars to online scammers. Since he was always frugal, this was out of character financially as well as morally. I am still appalled at the way scammers prey on the vulnerable, but I wish I had recognized just how vulnerable he was much sooner. — LACK OF MOTIVATION: I also wrote not long ago about how Tom stopped paying attention to lawn care. This same lack of motivation, in large measure, resulted in him no longer playing his trumpet (formerly a top priority for him). After he hurt his lip in a challenging concert in 2016, he received a detailed plan to help him heal and rebuild his muscle strength, but he never followed through. He still tells people he’s a professional musician; the sad truth is that he hasn’t practiced consistently since he hurt his lip nearly seven years ago, more than three years before his diagnosis. — ODD PERSONAL HABITS: One day, I found him laying a towel down over the bathmat as he prepared to take a shower. When I asked about it, he said he “had never liked to get the bathmat wet.” It took a while for me to realize this was a dementia behavior, not a longtime preference that I had somehow missed. I remember watching the final funeral he officiated nearly five years ago and noticing how he constantly licked his lips as he spoke. Today, I see (and hear) that behavior whenever he’s not focused on something else, such as when we ride in the car. — INABILITY TO PLAN AND ORGANIZE: I was heartbroken when Tom lost his job as a music minister, but when I think back, I’m amazed he kept it as long as he did. I am sure one reason he could was the wonderful volunteer who kept him organized and on track, but even with her help, his planning became more and more erratic. It takes a lot of organizational skill to set up a worship...
read moreSnapshots of Dementia: It’s Broken (or not)
(Andres Urena on Unsplash) Tom hobbled into the kitchen the other day, a man on a mission. “What’s wrong, baby?” “My Fitbit is broken,” came his gloomy response. “What seems to be the problem?” “It won’t show me the time anymore. It’s broken.” Tom can’t walk for exercise anymore, but he retains his obsession with his Fitbit. He can’t charge it on his own anymore either, but he wants to make sure it’s always ready for use. And when he accidentally switched it over to timer rather than clock mode, he felt sure it was broken. You and I wouldn’t come to that conclusion. But you and I, for the most part, are not people living with dementia. “Here, let me see it,” I said, reaching for the device. Of course, it only took a few taps and swipes for me to return it to clock mode. “Here you go! I got it working again,” I said as I gave it back. It makes more sense to go with his reality than try to explain the details. He took the Fitbit, turned, and walked back to his recliner, his dismay forgotten. Given Tom’s obsession, you’d think he would have been happy and grateful. But although he still expresses happiness and gratitude at times, he does not typically connect those to events such as this one. And in the short time before I returned the device to him, he may have forgotten about his “it’s broken” conclusion. In the days when I didn’t realize Tom was LWD, happenings and conversations like this confused and upset me. Why was he acting this way? The “personality changes” mentioned in lists of dementia signs and symptoms often look different with different people. I’ve heard and read many stories from others whose loved ones are LWD. Since I didn’t realize that some types of dementia initially (and most types eventually) have a behavioral connection, I thought some of Tom’s odd behaviors were just that—odd behaviors, mistakes, or misunderstandings. Looking back (yes, we know what they say about hindsight) I realize that some or all were symptoms of the evil lurking inside his brain. Here are a few more of the changes he exhibited some time before he had a dementia diagnosis: — PESSIMISM: Always an upbeat person, he became a negative one. In the same way the Fitbit was “broken,” the banking website was “messed up,” and his discipline of our “terrible” dog became unduly harsh. For someone whose world is becoming more and more challenging, it’s easy, even natural, to be negative. — APATHY: Tom had less and less interest in family birthdays, anniversaries, even special events such as a couple’s baby shower for our daughter and son-in-love. This was not because he didn’t care, but because he couldn’t. Before we knew he was LWD, this behavior hurt. And when we think about who he was compared to who he is now, at times, it still does. — INAPPROPRIATE ATTENTION TO WOMEN: Tom would ignore me but flirt outright with women in service roles, such as at the grocery checkout. I never heard him say anything sexual, but the fact that he largely ignored me and paid attention to other women bothered me, and I addressed it in our marriage counseling to no avail. He still...
read moreSnapshots of Dementia: The Longest Yard
Photo by Andres Siimon on Unsplash I’ve had it!” my friend said. “I’m so tired of doing everything around here! She used to care so much about having a nice home. Now all she does is sit in front of the TV.” His words about his wife, who is living with dementia, reminded me of a time in our lives in 2015—more than four years before Tom was diagnosed. He seemed more tired every night than he had in the past, and I wondered if he was aging prematurely or perhaps just differently than I. And I really wondered about his obsession with simple computer games. In the evenings or on weekends, he would sit in front of his laptop for hours, not watching TV or engaging with me, just playing the same game over and over. In the meantime, I was either doing housework or working on a freelance assignment or walking the dog or. . . you get the picture. But what I didn’t do was lawn care. Our house in Florida didn’t have much of a yard; a pool and lanai (screened porch) took up most of the backyard. Mowing the grass didn’t take much time, but throughout our marriage, Tom had never wanted me to take on that chore anyway. And since I’m allergic to almost every kind of grass, I never minded. Over the past year or so, he had done less and less with our yard. But suddenly, he wasn’t taking care of the lawn at all. We had no children left at home, so we couldn’t assign this chore to one of them. The grass that had almost taken over some of the beds around the lanai was growing again, and I just couldn’t take on this job too. So—long before I took charge of our finances and every other aspect of our lives—I contacted a friend who has a lawn business. He and his team quickly got our yard back into shape, all while Tom and I were out of town, then continued servicing the lawn every week. What should have seemed strange was that Tom never objected to nor seemed grateful for this plan. In the past, paying someone for something he could do would not have been his idea of a wise expenditure. But he never said a word. In fact, only a few months after I hired the lawn service, Tom sold our lawnmower for a ridiculously low price to a neighbor who needed one. I was amazed. Was he planning never to mow the lawn again? Now that I know that he was at least on his way toward LWD, I know he didn’t have a plan at all. His day job was consuming most of his energy, and he couldn’t organize his free time enough to include regular chores. Back when I was wondering if Tom had dementia, I never thought to look up his lack of interest in household chores as a sign or symptom. I wish I had, because I see descriptions such as “loss of initiative” or “difficulty performing familiar tasks” on lists like this. But back when I first noticed Tom’s disinterest in lawn care, dementia hadn’t yet hit my radar. In fact, as I checked to see when I first hired...
read moreSnapshots of Dementia: Time Out
(Unsplash) She nailed it. My friend, whom I can always count on to call ’em as she sees ’em, read between the lines when I wrote about my foolish assumption that I wouldn’t need an alarm on my freezer. In case you missed that post, I learned the hard way that an alarm is an excellent idea when your loved one is living with dementia. What my friend noticed, in her usual insightful way, was not so much the cost of the food we lost—although that was significant. Instead, she pointed out the time I lost: — Time spent checking all the food (some of which remained frozen, much of which did not). — Time spent throwing out the spoiled items. — Time spent mopping the floor. — Time spent scraping, wiping, and otherwise cleaning up the freezer. — Time spent shopping to replace the spoiled food. — Time spent working late to make up for the time I spent doing those all those other things. Dementia has many hidden costs—$321 billion a year in the U.S. per a 2022 analysis. But without a doubt, one of the greatest is time—for the family or whomever is caring for the person LWD. As the disease progresses, the time spent on the person LWD only grows. I feel blessed to have a profession in which I can, for the most part, set my own hours. When I first began working from home, one of my jobs required a regular schedule with half-hour or every-hour deadlines. I had to start by 8:30 a.m. at the latest and often worked straight through for many hours with only the smallest of breaks to check on Tom. Over the past year and a half, God has allowed me to make some major adaptations in that schedule, and although at times I need to write or edit a piece within a few hours, I generally have a much larger window of time. That’s huge because although Tom can still do some things for himself, my time-costs have risen in the following areas: LEAVING THE HOUSE: This aspect of our LWD life reminds me of when our kids were small and I had to allow extra time because invariably, a last-minute emergency would delay us. Our LWD last-minute emergencies include bathroom visits, retrieving forgotten items, closing doors left open, him refusing to leave until he finishes a game on his iPad, and more. INTERRUPTIONS: This time-cost has increased significantly in the last six months. I have rarely asked Tom not to interrupt me while I work (and if I did, he wouldn’t remember). So when he misplaces his reading glasses, his Chapstick, his remote control, or something else, he asks for help—often several times a day. When he can’t solve one of his word games, he asks for help—often several times an hour. SPILLS: I mentioned in my last post that these have become more frequent. At least once or twice a week, I clean up spills on the floor or elsewhere, all related to Tom’s dementia. This week, I removed, washed, and dried everything in our silverware drawer (including the liner) after he spilled coffee grounds throughout. Bonus: I made a small start on my spring cleaning! DOCTOR’S APPOINTMENTS: Multiple physical problems have...
read moreSnapshots of Dementia: Ch-ch-ch-ch-Changes
(Photo by USG on Unsplash) I have discovered that I am not the only dementia caregiver who doesn’t love the question, “How is ___________(person living with dementia)?” The reason we don’t love it is not because we don’t appreciate the interest. I love having people show concern for Tom. My caregiver friends and I have trouble with this question because of only one thing: There’s no quick-and-easy way to answer it—and the person who asks rarely has time for or interest in the long answer. I generally respond with something like, “He’s doing as well as he can, but the disease is progressing.” That is true, of course. But what is also true is that behind each of these changes lies one more piece of my broken heart in which I realize that what goes away never returns. When I first told the world via Facebook about Tom’s dementia, I called it a thief. I still think that’s one of the most accurate descriptors for this enemy that has taken so much from Tom and from our family. Here are some of the ways it has stolen from us in recent days—in other words, the behind-the-scenes changes when I say he’s doing “as well as he can.” GROSS MOTOR SKILLS: He stumbles more nowadays when he walks and has had lots of near-falls. Using the walker for his back/leg problems has helped keep him more stable. But using a walker when you are LWD can be a challenge because you forget to grab it when you get up—and sometimes forget that you use it all. FINE MOTOR SKILLS: Tom’s handwriting, never great, has gotten worse, although he can still sign his name when needed. He can still feed himself, but he is getting more and more clumsy, often spilling his coffee or knocking something onto the floor. The tremors in his hands don’t seem to have worsened, but the spilling has definitely increased. SPEECH: He still talks, but he sometimes forgets what he intended to say and frequently struggles with how to express it. A conversation with him includes many pauses and sighs. When he does connect his thoughts, he can contribute, but what he says may contain gaps in logic or reality. However, he can still insert a joke or wry comment with surprisingly on-point comedic timing. In a social situation such as a crowded restaurant, he usually shuts down; too much stimulation seems to overwhelm his thinking. MEMORY: This is one area that keeps changing, but the changes don’t always make sense. He can still (usually) prepare his own coffee, but sometimes he forgets what he is doing while making it, and later, I find his open mug and creamer on the counter. At other times, he remembers a scheduled event or something someone said that I didn’t expect him to recall. It’s as though his brain is a sieve, and I never know which thoughts it will catch. PERSONAL CARE: He can still take his own shower, shave, brush his teeth, and so forth, but I have to remind him about all of these, and he doesn’t handle them as well as in the past. We have grab bars in our shower, and he has used these on occasion to keep from falling. He shaves only about every three...
read moreSnapshots of Dementia: A Person’s a Person
(Facebook/Horton Hears a Who) You remember the Dr. Seuss story. Horton the Elephant becomes the champion of Whoville, going to extreme lengths to save its citizens from threatened destruction by his jungle pals. The theme that resonates throughout arrives in Horton’s oft-repeated line, “A person’s a person, no matter how small.” We’d all agree. Or would we? I used to complain—or at least wonder—about people who seemed unaware of those around them: How can they not pay attention to anyone except themselves? You’ve seen people like this. It’s the woman so focused on the groceries she needs that she doesn’t realize her cart is blocking the aisle. It’s the man who talks loudly on his cell phone, oblivious to the fact that he’s disturbing everyone around him in the otherwise-quiet waiting room. It’s the woman next to you at the beauty salon who launches into a long story as if you were her best friend, eager to hear all the not-so-interesting details. It’s someone living with dementia. Or at the very least, it could be. Tom, my person LWD, has trouble focusing on more than one thing at a time. He doesn’t push a grocery cart for me anymore, but when he did, he would often cut across someone’s path without realizing they were there. I intercepted several angry looks and gestures while he remained oblivious. He rarely uses his cell phone now, but when he did, he tended to speak loudly, and his conversations were often circular in nature. Since he couldn’t follow directions well, whatever was explained to him had to be repeated more than once, often without good resolution. And his stories? Most people who have even a passing acquaintance with him has heard at least one of his stories—often multiple times. Today, we visited a medical specialist’s office. It was our second visit, and although the doctor was treating Tom for a medical problem, he of course knew he is LWD. At first, the doctor spoke kindly to him. He even repeated himself without flinching when Tom asked about the same thing he had explained less than two minutes earlier. But the more time they spent together, the less patience this doctor seemed to have. By the end of the appointment, as Tom tried to finish a (surprisingly brief) story, he interrupted him, gave me some final instructions, and walked out of the room as if Tom weren’t even present. I know doctors are busy, and I know this one had other patients waiting. And Tom? He didn’t seem to notice anything had changed. He blinked, turned his attention to me, and promptly forgot what had happened. But I knew. And I won’t forget. At my next opportunity, I’ll speak a few words to the doctor about the respect I feel a person LWD deserves. I’ll do so because: • A person’s a person, no matter how small their IQ. • A person’s a person, no matter how short their memory. • A person’s a person, no matter how many times they ask you the same question. • A person’s a person, no matter how rude. • A person’s a person, no matter how confused. • A person’s a person, no matter how much extra time they take. When we meet...
read moreSnapshots of Dementia: Scam Alert, Part 2
James Wheeler/Unsplash “What I would really like—is to have my Facebook back.” It took Tom a much longer time to get those words out than it used to. But when he said it a few months ago, my answer didn’t change. I’ve heard this request a few times since, at the request of our marriage counselors, he closed his Facebook account in 2018. I am far from a control freak. And the reason I will never say yes to this request is not so much because I’m worried about what he might post—if he could—but because that’s how the scammers initially found him. Like many of us, Tom loved connecting with friends on Facebook. And eventually, scammers loved connecting with him too. I’m not sure how they initially found him, and doubt I want to know. But I do know that those villains I’ve learned are called “catfishers” got him, and through Facebook and email, they hooked him. All through one summer and part of the fall, he was giving away money in the ways I mentioned in my last post. When I opened separate bank accounts, I wasn’t trying to keep him from our money but to protect it. Raising five children on a pastor’s salary plus my varying freelance income, we’d never had a lot extra. I had intended to use my now-regular income as savings for retirement. Instead, I had to pay off his huge credit card bills—and pay back our children’s college trust. That fall, our marriage counselors asked Tom for an accounting of how much he had given away. I’m not sure he remembered it all. But with what he could account for, the total came to nearly $30,000. Had I not found that final uncashed check, it would have been at least $10,000 more. Because the doctors still kept telling us he was fine, neither our counselors nor I associated his behavior with dementia. Serious problems, yes. Dementia—no one else seemed to think so, so why should I? At least four times, Tom fell for scams as believable as the emails we’ve all gotten from the wealthy prince in Nigeria. Despite his interest in other women, his primary motivation was helping others. Even when, through counseling, I gained the strength to insist he stop contacting the catfishers or move out, he at first insisted he needed to keep his one remaining contact. After all, she was stuck in another country with no way to get home, and “she promised to pay me back.” The few times I’ve shared even part of this story, people ask if we ever recouped our money. Not. A. Penny. Tom went to the police early on to complain about being blackmailed, and whatever they said convinced him there was nothing we could do. I don’t think he even realized the others were also scammers. Since I knew he had willingly given up the funds and, at the time, didn’t know he had dementia, I never considered seeking legal help. It was all I could to hold my life, my job, and my marriage together; I didn’t have time or energy for much else. And I didn’t know there was an National Elder Fraud Hotline for schemes just like what we experienced. Despite the financial losses, I can say without a doubt that gains came too. The counseling...
read moreSnapshots of Dementia: Scam Alert, Part 1
(Unsplash) “Turn it off,” I said, my voice shaking. “I just can’t watch that.” The YouTube video that caused me to speak to my daughter in such a direct way had a topic too familiar to all of us: dementia. As I recall, it involved two men who exposed scams, this one targeting senior adults who were living with dementia. The investigators were doing a great job of ferreting out those responsible and (I presume) helping bring them to justice. That wasn’t the problem, of course. The problem, for me, was the deliberate way they pointed their attacks toward someone LWD, easily confusing and misleading them. And the real problem—the reason I couldn’t watch anymore—was that this happened to our family too. More than two years before Tom’s official diagnosis with dementia, while the neurologist was still telling me he was fine, we experienced one of the worst seasons of our lives. We were already going through marriage counseling after he confessed some very inappropriate activity (not a physical affair). What should have been one of our happiest times, with one of our daughters getting married that summer, quickly become just the opposite. Tom was barely doing the required homework for our marriage counseling. In fact, he often seemed disinterested when we met (via Zoom, although the pandemic was a few years away) with our counselors from Pure Desire Ministries. The loneliness I often experience now while married to someone LWD is nowhere near as great as what I felt then. I cried nearly every day, sometimes sobbing for much of my forty-minute drive to and from work. Why did my husband no longer seem to care about our marriage? Over that summer and fall, at the same time as we were going through counseling, complete with accountability partners to whom Tom reported every week, he was giving away our money, several thousand dollars at a time. The first time, while out of town, he had money wired from our bank to share with a scammer. Later, he used credit to buy gift cards, also shared with a scammer. And here’s one of the worst parts: because he was the primary money manager, I had no idea any of this was happening. I had noticed his increasing struggles, and (at my insistence) Tom had a neurological workup including an MRI, but I wasn’t yet in relentless pursuit of a diagnosis. In fact, it took almost a year after that for me to connect the problems in his behavior and in our marriage to his dementia. Like many people, I thought of dementia as primarily a memory issue. Tom had some memory problems, but he also had many other behavioral symptoms that he still exhibits today. Even way back then, while he was still holding down his full-time job as a worship pastor, he showed symptoms such as apathy, obsessive behaviors, hiding and hoarding items, and an increasing lack of logic and planning ability. It seems so obvious now, when I can look at a list of behavioral dementia symptoms and recognize how well his fit the pattern. But back then, some of his actions upset me so much that I don’t know if I could have put it all together even if I’d known more. The financial concerns came to...
read moreSnapshots of Dementia: My Favorite Things
(Screengrab, “My Favorite Things,” YouTube/Fox Family Entertainment) When Julie Andrews sang it, it sounded like so much fun: “I simply remember my favorite things/ And then I don’t feel/ So bad.” When you are living with dementia, can’t think much beyond the moment, and have a memory that grows shorter by the day, you remember your favorite things—and stick with them. In Tom’s case, as in the case of many people living with dementia, the familiar and favorite have become the essential. For him, “favorite things” include: Music: Since Tom was a professional musician and worship pastor, music comes first. Although he doesn’t listen to music as often as before he was LWD, he still loves it. He owns about 30 Christmas CDs, but this year, he played only two—multiple times. If you get him talking about jazz, he’ll want to share YouTube clips of favorite bands, although he’ll need help to find them. His smaller memory has compressed his list of favorites, but he still knows what he likes. Radio: Tom has a regular weekday and weekend morning regimen of radio programs. We’ve lived in South Carolina for more than three years, but he still insists on streaming the same Orlando NPR station he enjoyed on his morning drive to work. On Saturdays, after he’s finished with the NPR lineup, he listens to children’s programs on a California station—the same one we listened to every Saturday when we lived in Oceanside many years ago. Television: His television tastes vary a bit more than his radio ones, but not much. For a while, he would watch repeated clips of The Carol Burnett Show and a few other childhood favorites. For the past couple of years, he’s only watched a few new programs. We’re now on the fourth round of one of his favorite shows, Blue Bloods. He enjoys the repeated episodes as if watching them for the first time—because with such a short memory, he is. Books: With my help, Tom still checks out books from the library, reading mostly digital books on his iPad. As with television, he understands largely in the moment and can’t often explain or describe the content. Except for his morning Bible reading, he doesn’t read every day, and he reads and rereads only a few favorite authors and books. Electronic Games: Before his diagnosis, I despaired of the time he spent playing what seemed like mindless games on his laptop. Now, he plays games on his iPad, mostly a golf game he’s enjoyed for years (although he now plays at a much lower level) and a series of word games (with frequent help from me). These all cause a certain level of frustration, but he returns to his favorites every day. Clothes: If I weren’t watching, I’m sure Tom would wear the same clothing all week, partly because he would forget to change and partly because he prefers his favorites. I still choose my battles and don’t insist that he vary his wardrobe too much, but after discovering that he often hangs up dirty clothes, I keep a watch on the closet. Foods: These range from Wendy’s Frostys to cheeseburgers to his beloved coffee. He doesn’t get upset when I switch up our menu, but the most familiar remain his favorites. The biggest change while LWD is that,...
read moreSnapshots of Dementia: The Kindness of Strangers
(Unsplash) “You can’t leave that sticker on a package.” The postal clerk across the counter from me may not have meant it as a rebuke, but nonetheless, I felt scolded. “It tells us the contents are dangerous, and we can’t let it go on a plane.” I knew right away what she meant. After I’d sealed up my package (a recycled box from the company that promises to deliver smiles), I noticed some stickers left over from its previous use. I pulled off the ones I could and used a black marker to scribble over the others. Good enough, right? Wrong—as my postal clerk friend had so quickly informed me. Great. Just great, I thought. I’m not only late sending this off to Mom, but now I’ll be even later. I knew the “danger” sticker lay under the package-sealing tape I’d used on the box—the roll of tape that remained at home, along with the tools I would need to remove the tape and sticker. I moved to reach across the counter and retrieve my box, but the clerk had more to say. “If it can’t go on a plane, your package won’t get there when it’s supposed to.” I get it, lady, came my somewhat uncharitable thought. I know what I need to do. Please, just let me take it home. But no, she had still more to tell me. “Here, let me try to take it off for you,” she offered. “There’s no reason for you to have to go all the way home.” What? Kindness? I wasn’t expecting kindness—especially when I’m the one who made the mistake. She tugged at the edge of the offending sticker, ultimately getting out a pair of scissors to unseal the package, then using her fingernails to pick at the sticker until all the pieces had been removed. Shen then pulled out a roll of tape, resealed my box, and prepared to send it on its way. “I really appreciate you taking the time to do this,” I told her. “My husband has dementia, and I’m his caregiver, so it’s a big deal anytime I can get to the post office. Thank you so much for taking care of this so I don’t have to make two trips.” “I’m so sorry,” she said. “I was a caregiver for my husband for five years before he died.” She had more words for me about the stresses of caregiving while she finished getting the package ready for its journey. All this took a few extra minutes of her time—minutes she may not have had, considering the busy-ness of the post office—and I appreciated her kindness so much. “I never do those [USPS] surveys,” I told her as she handed me my receipt, complete with the opportunity to participate in a survey. “But I’ll do one this time and mention how kind you were.” “That’s nice of you, but really, don’t worry about it,” she said. “But I want to.” “Well, if you get home and you don’t have time, just forget about it. I know what being a caregiver is like.” And then she gave me a final word that seemed unusually thoughtful: “I’ll keep you in my prayers.” I didn’t find time to do the survey for a few...
read moreSnapshots of Dementia: Resist the Urge to Explain
Gerd Altman on Pixabay My fellow writers will know what I mean by RUE. Our writing bogs down when we explain rather than letting a story happen. As we grow in our work, we learn to Resist the Urge to Explain. As with many parts of my life, I’m finding connections for that rule with dementia too. More and more, I resist the urge to explain. And as with many parts of my life, it’s not always easy. When Tom and I were newlyweds, his extroverted personality and penchant for embellishment often resulted in him telling a story (sometimes in a sermon) that, for me, pushed the boundaries. I came to understand that he was telling the truth as he saw it, which often looked very different than it did to me. Now that he is living with dementia, the difference between our viewpoints has grown even more profound. His physical sight is changing—he can look right at something and miss it—but so is his perspective, the way he interprets the world around him. At an earlier point in our dementia journey, he had trouble remembering recent events but not those from the past. He could tell stories from his college days or the early years of our marriage almost perfectly. In fact, he sounded more “himself” when sharing these old stories than at almost any other time. Now, he still tells stories he’s told many times, but they sound different. He often puts pieces of one into another or mixes up the details. It bothers me to hear these stories—many of which are my stories, too—with people, situations, and circumstances shifted around, left out, or otherwise changed. I find myself listening to his story with one ear and telling myself the true story with the other. But ultimately, those details don’t matter. I’m learning to resist the urge to explain. I still try to let Tom do the things he can do. But this tendency to see an alternate reality can make that challenging. We faced this problem a few months ago when I realized he had been calling the wrong barbershop. We would arrive for his appointment and find the shop closed or the owner with no record of his call. It took about three rounds of this before I realized what was happening, and he still made one more appointment at the wrong shop. I only caught it when I heard a male voice responding to his call (the barbershop he prefers has only one barber, a woman). Once again, his reality looked different than mine. As much as I want him to carry out the tasks he can, he just can’t make appointments anymore. But I still let him go in for his haircut on his own, carrying cash I give him right before he enters the shop. And I resist the urge to explain. Yesterday, when he spilled his coffee all over my newly mopped floor, I told him, “We need to go pick up your travel mug.” The missing mug has a top with a mouth that seals shut. He left it in a nearby church where we’d rehearsed for our Christmas musical. Although I’d emailed to ask about it, I’d never taken time to retrieve it. In its absence, he...
read moreSnapshots of Dementia: Sudden Impact
(Paul Barlow, Pixabay) For much of this year, we’ve rocked along in our dementia journey without major obstacles or downturns. In fact, I realized the other day that Tom hasn’t had a major fall for a number of months. I don’t know if we can attribute that to an improvement in his balance, to his now-regular use of a walker, or to something else, but I’m grateful. However, I do recognize that his general direction is not up or even forward but steadily downward. At times, the force of what’s happening slams me right in the face—or, more accurately, in the heart—with what I can only describe as sudden impact. This happened just two weeks ago when we were rehearsing our Christmas presentation. During our rehearsals, my mind kept returning to only a few years ago. Every December, Tom would throw all of his musical, physical, and spiritual energy into directing a full-blown Christmas production. Yes, I was proud of and grateful that this year, he sang a solo. But when I allowed myself to compare that to everything he used to do, the tears threatened to overflow. As we presented the Christmas music for the audience, I asked God to help me concentrate on the music, the message, the moment—so I could rejoice rather than weep. And thankfully, Tom never knew anything otherwise. Another sudden-impact moment happened just last week when a research coordinator from Emory’s Neurology Department met with him via Zoom to conduct some cognitive testing. In the past, doctors used these tests to help determine their diagnosis (or, for years, their lack of one). Now, the tests help assess how his dementia is progressing. Some relate to memory, and others, to overall cognition. When we were desperately seeking diagnosis, I wanted the testing to reveal deficits. Back then, his scores were high, remaining in the normal range even when his behavior showed obvious problems. But during last week’s testing, I realized that I wanted him to remember more or perform better than he could. The sudden impact came when I realized he couldn’t follow the simple instructions for some of the tests. Of course, I had to connect my laptop to the internet and set up the Zoom call; that would have been far more than he could do. In the past, Tom refused cognitive testing once or twice because he had taken these tests so often. Now, he simply accepts it as something he’s supposed to do—one more event that came with a sudden impact. We don’t have the full report yet, but the preliminary notes said the testing showed deficits in multiple areas. This shouldn’t have been news, but I still felt its sudden impact. This week, I experienced yet one more sudden-impact moment. For the past few years, Tom has enjoyed watching The Voice. The combination of musical talent and silliness fits his interests and attention span well. This season’s finale took place Monday and Tuesday, but we only watched part of Monday night’s show and none of Tuesday’s. Tom still likes to control the remote (raise your hand if this surprises you), although he needs more and more help to use it appropriately. We waited until tonight to watch Tuesday’s final episode, but he clicked on Monday’s night’s show. I knew...
read moreSnapshots of Dementia: Do Hard Things
Do hard things. So reads the plaque on my office wall, courtesy of my two former “work daughters.” That phrase became our mantra as we learned that God often calls us to the more challenging choices, those more difficult, more sacrificial, and often, more right. He calls us to do hard things. For me, that sometimes means handling insurance, tax, or other details I’d prefer to ignore. Sometimes it means interrupting my work multiple times a day to help Tom with a word game or find a (temporarily) lost item. Sometimes it means taking on yet another household task he can no longer perform. And sometimes it means helping him tackle a challenge I’m not sure he can handle. In the past, if such a situation occurred while I was raising children, I might have said I was giving my child the freedom to fail. But Tom already experiences small failures multiple times a day. When I help him do hard things, I’m giving him the freedom to succeed—even if success doesn’t look the way it used to. For most of his working life, Tom served as a senior pastor, then a worship pastor/minister of music. He also played his trumpet professionally for churches and other venues. As a worship pastor, he planned and directed a number of Christmas productions, some with three performances per Christmas season and components including drama, lights, and sound as well as choral work. This year, when our worship pastor announced that our choir would combine with two others for a community Christmas presentation, I felt both excited and sad. The music came from one of Tom’s all-time favorite arrangers, but the production was shorter and less complicated than the ones he had directed. Yet as I read over it, I knew it might still be too much for him. I wondered about his physical ability. I knew he wouldn’t be able to stand for much of the time, but I also knew that, just as he used to tell his choir members, it would be fine if he sat. I wondered about his emotional ability. How hard would it be for him to “only” sing when, just a few years ago, he had directed similar productions? I wondered about his cognitive ability. During our regular choir practices, I’d noticed him struggling to follow along with his music at times. How would he handle this more difficult score? Tom accepted the idea of the Christmas production well—not enthusiastically, but he rarely shows enthusiasm anymore now that he is living with dementia. Before long, he told me he wanted to try out for a solo. What? I’m wondering if he can even sing in the choir, and now he wants to do a solo? That was my first thought. My second thought—after getting an enthusiastic response from my minister of music when I asked for his input—was a resolution to do hard things. And to help Tom do them too. What did this look like? — Helping him choose which solos he might attempt and receiving/downloading the tracks so he could learn the parts. — Reminding him/helping him practice both for the audition and for the program—and rejoicing with him when he was awarded a small solo. — Reminding him of specific words in...
read moreSnapshots of Dementia: Above and Beyond
Unsplash It’s an ordinary bank, and she was an ordinary teller. One of thousands of ordinary others, paid to do an ordinary job in an ordinary way. Or that’s what you might think if you didn’t know the full story. For a while after we moved to South Carolina, I kept my Florida bank. Changing banks is a hassle, especially with the multiple responsibilities I have, and I could do everything I needed with the mobile app. Everything, that is, until the Social Security Administration said I had to have a separate account for Tom’s finances once they said he qualified for disability funds. Since his disability diagnosis related to his dementia, they wouldn’t release the funds until he had a representative payee (which they recommended be me) in place. I did a little research and decided on a local bank, made a visit, and explained my situation. The customer service representative helped me open the appropriate accounts and later, a business account that I needed as well. Because of working as a freelancer, I don’t have many automatic deposits to my accounts, and I often have deposits that exceed the limit for the mobile app. This means I make at least two or three trips to the bank every month. I try to go when Tom is settled in his recliner and busy with his iPad so I don’t have to upset his routine. Generally, I can get to and from the bank within fifteen minutes, give or take (advantages of a small town). Just an ordinary trip to an ordinary bank—until one ordinary teller made those trips extraordinary. Not only did she quickly learn my name and greet me with a big hello every time I pulled up to her window, but she knew my car (and when I changed vehicles this year, she recognized the new one too). She always asked how I was doing, and she always seemed interested in my answer. Early in our relationship, I told her about my husband’s dementia, and she often asked how he was. When I brought him along and introduced him from his seat on the passenger’s side, she was just as kind to him as she was to me. She also told me about herself. When she took a vacation, I heard about it (we share a love for the beach). We talked about the seasonal decorations in her bank window; she enjoyed setting up little scenes so it “wouldn’t look boring” for people in the drive-through. Of course, we only spent a few minutes together at each visit, but (especially during a season when Tom didn’t feel like going to church) sometimes talking to her was my only in-person interaction with someone other than Tom for a number of days. I’m sure she didn’t know how lonely or starved for “normal” conversation I felt. I’m sure she didn’t know that I deliberately chose “her” lane every time I came to the bank— even when the other lane was empty and I had to wait in hers. I’m sure she didn’t know how much I looked forward to the simple act of making a deposit. And I’m equally sure that she didn’t know that I wiped away a few tears when she told me this...
read moreSnapshots of Dementia: Pro Tips
Big things can hurt us—a heart attack, a broken bone, a dangerous diagnosis, the loss of a friend or family member. But little things sometimes hurt us too. Here are some of the big little things we’ve encountered this week in our dementia journey—and a few tips I learned along the way. Time Change: When our oldest kids were toddlers and Daylight Saving Time ended, we would tape black plastic over their windows to try to ensure better sleep for the first week or two post-switch. Most of the time, it didn’t work. I’ve felt tempted to do the same this week, because when we “fell back,” Tom didn’t. He’s gotten up at 4 or 5 a.m. most days this week, and since I tend to stay up for a while working (or writing this blog) after he goes to bed, I’m worn out. PRO TIP: If you’re caring for a partner who is living with dementia, going to bed when they do—as long as it’s not, say, right after dinner—makes a lot of sense. It’s always easier for the person who is not LWD to change their habits than for the person LWD to do so. As a lifetime night owl, I know I won’t do this every night, but I’ll try. Again. Feeding Frenzy: Near the beginning of the week, I made two small coffee cakes. I found fresh blueberries on sale, and this recipe is one of Tom’s longtime favorites. That’s why I was surprised when, after a couple of days, he hadn’t eaten any. “I made your favorite coffee cake,” I told him. His answer also surprised me: “I have to eat my cereal.” “Couldn’t you eat coffee cake too?” I asked. He didn’t respond, which either means he didn’t understand or couldn’t process an answer before he forgot my question. But I soon figured out what he meant. We had recently bought multiple boxes of Chex (three kinds in one giant package). Tom loves Chex, and he happily placed four huge boxes of it in our cart at a club store not long ago. I bought it because, although we don’t really need so much on hand, it’s better for him than many other kinds of cereal, and I knew it would keep. I realized his mixed-up, LWD logic was telling him it was more important to eat the cereal than the coffee cake. People LWD lack the logic that would say homemade coffeecake spoils much more quickly than processed cereal and fresh baked goods taste much better than older ones. In Tom’s world, “I have to eat my cereal.” I wrapped up one coffee cake and froze it, sharing some of the other with a friend and grateful to have navigated his illogical logic. Of course, even though “I have to eat my cereal,” he ate a giant piece of coffeecake that afternoon and has now finished it all. PRO TIP: People LWD often lack logic. What makes sense to you may not make sense to them, and vice versa. Choose your battles. And if you really need that coffee cake to disappear, hide the cereal! Schedule Swap: As a homeschool mom with five children at home, structure and order were my friends. I learned not to let the schedule run our lives, but in general, a good routine helped our days go well. Now that I’m...
read moreSnapshots of Dementia: Learning the Hard Way
(Pixabay) As the mom of five children, I’ve said more than once over the years that one or more of them “had to learn things the hard way.” Sometimes I chose not to tell them what I thought was a useful, even essential piece of information because I realized they wouldn’t receive it. At that point in their lives, I knew they had to learn things the hard way. And—like many of us before them—they did just that. After all this time, I’ve discovered, much to my chagrin, that I’m also someone who has to learn things the hard way. We have an upright freezer in our garage. A few months ago, Tom forgot to close the freezer door, and we lost several cartons of ice cream before I discovered it. “Mom, you can get an alarm for the freezer,” my son told me. “It would let you know whenever the door was standing open.” “Oh, I don’t think we need that,” I said. Especially because of Tom’s memory loss, I have often appreciated the alarm on our refrigerator door, but a garage alarm seemed like overkill. I could always check on the door after Tom used the freezer. And he didn’t go out there too often anyway. Why spend the money on an alarm? You guessed it. He left the door open again a few months later. This time, I caught it fairly soon and closed it before any food was damaged. And it happened again—because a box fell over and held the door open after I used the freezer. This time, I had to wash and replace everything on the door and a few things inside the freezer too. But I still didn’t buy an alarm. It was my mistake, I reasoned. I’ll just make sure no boxes get in the way. I carefully cleaned and rearranged the entire freezer before filling it up again. I found myself checking and rechecking the door whenever one of us used the freezer to make sure we had no further problems. After all, I didn’t want to go through the mess or expense again. Ice cream remains one of Tom’s favorites, and as with most of his comfort foods, he feels much more secure if we have plenty on hand. This means we keep six or eight cartons of ice cream in that outside freezer (he doesn’t think they stay cold enough in the freezer at the bottom of our refrigerator). Years ago, I got into the habit of buying meats and other items ahead of time, and I also freeze soups, homemade pizza crusts, and other meals or ingredients so I don’t have to cook every night. In other words, we make good use of our freezer. Except when we don’t. Except when Tom gets himself some ice cream while I’m working late one evening, and I don’t think to check the freezer. Except when the door stays open a few inches all night long. Except when I don’t notice the open door till I’m putting the trash out the next morning and realize that, once again, we have several cartons of ice cream soup on the door and more of the sweet sludge in the bottom of the freezer. The other day, I posted a meme expressing my thanks for the...
read moreSnapshots of Dementia: Thank You for Being a Friend
Tom with longtime friend Marty Marks, who drove across several states to visit us in 2020. Tom has always been a relational person. One of the things he taught me early in our marriage was to value people. Through the years, we have traveled many miles, often out of our way, to spend time with friends. In a marriage that has taken us coast to coast, we rarely lived close to our biological families, but God has consistently given us friends who have become family. The onset of COVID gave us a somewhat rough landing in our then-new hometown—but the delays caused by lockdown have made us appreciate relationships even more. Every time we’ve gone through a challenge in our lives, we’ve noticed that the true friends remain. The same has proven true of dementia. I read this week that one in ten U.S. adults over age sixty-five now has dementia. And then there are the many, like Tom, who develop it well before that age. In other words, you most likely know someone living with this disease. So how can you be a friend to someone living with dementia? Based on the thoughtful ways his friends and family treat him now, here’s what I believe Tom would say in response to this question if he could. NOTE: This is by no means an exhaustive list and will vary from person to person. It will also change with disease progression. 10 WAYS YOU CAN BE A FRIEND TO SOMEONE LIVING WITH DEMENTIA 1. Talk to me—and listen to what I say. Social situations challenge me, but they also help me. 2. Touch me. Physical touch still matters to me. Feel free to hug me, take my hand, or whatever is comfortable and appropriate for our relationship. 3. Remember that I forget. Try not to ask, “Don’t you remember …?” even if it’s about something that just happened. The short answer: No, I don’t. 4. Forgive me. I don’t have the same control over my emotional responses as I did in the past. I may cry, laugh, get angry, or fail to respond at all in situations where you might expect just the opposite. 5. Move on. I may do or say things that are at best awkward or repetitious and at worst inappropriate, even offensive. A wise friend will ignore whatever I said. If you move on, I will too. 6. Be sensitive. Respond to the me you see today, even if it’s different than the last time we interacted. My cognitive state and behavior depend on my physical health, time of day, and a number of other factors. 7. Respect me. Allow me to do those things I am still able to do, even if I don’t do them well. Remaining active helps both my brain and my body. 8. Let me be quiet. If I’m silent, there may be too much happening around me, and I can’t process it fast enough to respond. 9. Protect me. While my thinking process and even some of my physical abilities have changed, I don’t always recognize it. If I’m endangering myself or someone else, please either speak to my care partner (if immediately available) or redirect me. 10. Recognize me as a person of worth and value, created in...
read moreSnapshots of Dementia: Tired Out
Photo by Chris Saur on Unsplash I anticipate this being a short post because, well, I’m tired. That description still applies to me too often, but I know it also applies to many of my fellow care partners—for all sorts of reasons. Some of my exhaustion is my fault. I make choices, such as I did today, to do outside activities with Tom. But taking time off during the day usually means I have extra work to do in the evening. As a normal part of our evening, I walk after dinner while watching TV with Tom. We used to walk outside, but his leg and back pain make that impossible right now, and I can’t leave him alone while I walk. Still, he’s happy to share something he enjoys with me, and I’m happy to keep up my steps. Tonight, I stopped walking at about 9 and came back to edit some articles—and still had this blog to write. Tom went to bed about 9:30, so I had to stop, give him his medicine and help him get settled for the night. But I digress. Probably because, well, I’m tired. For more than two weeks now, Tom has fallen into a pattern of waking up early—”late” for him right now is 5:30 a.m—and not going back to sleep. Sometimes he’s gotten up as early as 3 a.m. Sleep disturbances have become a regular part of our dementia journey. Tom has taken medication to help him sleep since soon after diagnosis, and we’ve added/changed medications (prescriptions along with melatonin) here and there in response to episodes of extreme unrest. This is the third time in 2022 that we’ve gotten into a cycle that has him waking up earlier and earlier. That gets complicated for several reasons. If he wakes up early, he tends to nap later on. When he naps, he’s not as tired at night, so he wakes up early again the next day. You get the picture—and well, I’m tired. I’ve also become a light sleeper now that I’m a care partner. Much like a mother with a newborn, I keep one ear out for Tom and almost always know when he gets up to use the bathroom or to stay up. I listen to make sure he’s settled into his recliner. So far, he hasn’t tried to take a walk, eat, or even make coffee when he gets up early; he simply goes to his recliner and starts his morning routine of reading his Bible, playing games on his iPad and, when it begins, listening to “Morning Edition.” (Interestingly, although we’ve lived in South Carolina for nearly three years, he prefers the Orlando public radio station he listened to when we lived in Florida—a comfort-zone behavior like the others I’ve mentioned here and there.) When you have dementia, you live more and more in the moment. Living in the moment means you rarely think, Oh, I should be quiet. My wife is trying to sleep—or, if you do, you don’t have the capacity to be quiet. Although he does play the radio at a low volume, he doesn’t realize that activities such as opening and closing drawers or leaving lights on will bother me. Today, he did something he rarely does anymore and went...
read moreSnapshots of Dementia: What I Wish I’d Known
Photo by Aaron Burden on Unsplash What is something that you wish you’d have known early on, or wished you’d have done or put in place? A woman whose husband is newly diagnosed with young-onset dementia, early stage, asked this question of other spouses/caregivers, and it moved me to think—and now, to write. That’s part of the reason behind my blog, I thought. But her question also prompted some specific responses. 1. I wish I’d known more about dementia early on so I could have pushed sooner and harder for a diagnosis. No (because some of you will think this), I’m not beating myself up. You can only know what you know. But if I had understood sooner that dementia encompasses much more than memory problems, and especially that it can have various effects even while the affected individual still performs well on standard cognitive tests, I wouldn’t have accepted the “No, he doesn’t have dementia. Come back in a year” responses that I heard for more than two years. 2. I wish I’d known that dementia would change more than Tom’s mind and memory. Even before he was diagnosed, I noticed that he had lost his sense of smell, although I didn’t know that was a common symptom of dementia (no, not just of COVID-19). I noticed some obsessive behaviors. I noticed him having increasing trouble finishing tasks he started. I noticed him withdrawing from family and failing to initiate conversations. And I noticed a whole host of other problems, many of which I’ve written about on this blog, that I never knew had a thing to do with dementia—but they did, and they do. 3. I wish I’d known the true value of narrative. Although I make my living from story, I dismissed its worth. Neurologists and others want and need objective ways to measure symptoms and determine diagnoses, and I understand that. But I also believe strongly that they must consider reports from the individual and (because many people living with dementia, or LWD, often have, as Tom did, anosognosia, a lack of awareness of their symptoms) from those closest to them. Early on, the most supportive doctors we had were the ones who listened and took notes on what I reported. The least supportive were those who dismissed my concerns because the objective testing did not at the time support our subjective experience. And yes, the objective matches the subjective now. But why did we, and why do so many others, have to wait until their loved one is midstage in the disease before medical personnel will agree that there’s a serious problem? 4. I wish I’d known how many others were trapped in the same sea of uncertainty as we were. Since beginning this blog, I’ve had many people comment publicly and write me privately to tell me of their similar experiences. I write not out of some deep inner desire to spill my (or my husband’s) stuff or, in effect, to share the bad news. If what I share can help even one person move one step closer to asking the next question or making the next appointment or doing the next right thing, the time and words I share are worth it. And I’m grateful that God has shown me, again and again, that these...
read moreSnapshots of Dementia: Sadness, Slowly
(Image by Mylene from Pixabay) I hope this blog gives you as many hopeful, joyful snapshots of dementia as sad ones. But as I sit, alone again, in a quiet house after Tom’s early bedtime, I’m thinking of a term my dear friend and fellow writer Tracey Pratt taught me: anticipatory grief. That’s typically a type of grief that occurs before someone dies, sometimes (as in Tracey’s case with her only daughter) years before the death occurs. As she worked on the initial chapters of her book on the topic, Tracey taught me that anticipatory grief is a genuine and difficult emotion, and each person’s journey is “unique, normal, and significant,” as she puts it. What neither she nor I knew was that I would, all too soon, experience anticipatory grief myself. I remember the weight of shock that slammed into me when I read that dementia often results in death. Before dementia touched our family, I saw it as something that often happened as people moved toward the end of life, but I never thought of it as a killer. Although it’s very possible that Tom could die of something else, the various types of dementia are considered terminal. The destruction they cause to brain and body can and will ultimately result in death. Learning, understanding, and living that truth over the past few years—especially while Tom remains largely unaware—has resulted in our family’s experience of anticipatory grief. The sudden loss of a spouse hurts. I have two close friends who have had that experience in the past few years, and I’ve watched their gut-wrenching grief. But losing a spouse bit by bit hurts too. Although our family has had some wonderful times to celebrate since Tom’s diagnosis, we’ve also had some times of deep pain. I say “we” because, as you could tell if you read our son’s recent post, Tom’s dementia hurts our entire family. My father died more than ten years ago, but like many others who mourn the loss of a loved one, I still get hit with a wave of grief when something reminds me of him. This happens with anticipatory grief too. Some of my recent, silent grief-moments include: —Listening to Tom ask me how to spell a simple four- or five-letter word and wondering how much longer he will be able to play the word games he still enjoys. —Taking over one more simple task because there’s one more thing he can no longer do and wondering, What next? —Hearing Tom get hopelessly off-track as he shares his thoughts in Sunday school and wondering how much longer he’ll enjoy the class at all. —Seeing his delight over the smallest pleasures—a dinner he enjoyed, a joke that made him laugh, a victory in his online golf game—and wanting to give him many more special moments. —Hearing Tom get suddenly agitated and loudly critical about a mistake at a community choir rehearsal and wondering if it’s time to stop attending. —Seeing our brand-new grandson, only hours old, for the first time over video chat and noticing how Tom barely looks up from his iPad. —Watching Tom in person with that brand-new grandson and wondering how much of his grandpa this little boy will get to know. Anticipatory grief is real. While not dwelling on it, I...
read moreSnapshots of Dementia: Trumpets and Touchdowns
by Andrew Pieper The Ohio State fight song rang out across the soccer field as hundreds of band members marched in unison, performing the iconic Script Ohio a mere fifteen feet in front of my dad, who sat on his walker, smiling and tapping his hand to the beat. Dementia has stolen many things from him: walking without pain, remembering what we were going to do that day despite having the conversation several times before, even constructing sentences at times now proved difficult for one of the most intelligent and humorous human beings I’ve had the privilege to know. Indeed, the list of things that are different with my dad is much longer than the things that have stayed the same over the span of the past few years. However, one of the things on that short list is music. He hasn’t lost a beat, literally. His doctors told us music will probably be one of the things he keeps the longest, simply because it’s been such an integral part of his life for so many decades. Upon hearing this news a year ago, I decided to buy a trumpet and take up playing again after giving it up in middle school, and we’ve been able to practice and talk music together. It’s really something to see how often on my weekly video chats with my parents, my dad is quiet and disengaged, but if I start talking about music, he instantly comes back. One time, I was describing a song, “So it goes A, A, B, C . . .” and without having any music in front of him, he corrected me right away, saying “Oh, that B is a B flat.” He just knew because it’s part of who he is, just like tapping his hand to the beat of the band. It wasn’t something conscious; it’s just part of him. We had driven over 500 miles across five states for this: to see the pride of the Buckeyes, the Ohio State University Marching Band, practice and then perform in a primetime game on a clear Saturday evening. (My mom is the Ohio State graduate, but Dad and I have become equally big fans.) I had emailed earlier in the week with Christopher Hoch, the band director, asking him what I should do to provide my dad with the best music experience possible. He was very gracious, telling me the time and place where they practiced and what to expect on game day. It wasn’t the easiest trip. From constantly reminding Dad what time we were doing things to changing out pain patches on his back, I devoted my full-time attention to making sure he had everything he needed to be safe and comfortable. Despite parking as close to the stadium as possible and arriving several hours prior to kickoff to beat the hundred thousand-plus fans coming to the game, it was still a long walk to the stadium. But I’ve found worthwhile things rarely come easily. As the band practiced in front of us and I walked around taking photos and recording video, I was having a hard time getting a clear picture. It wasn’t my camera or the lens; that image was crystal-clear. The vision problem was with me as tears of happiness welled...
read moreSnapshots of Dementia: ‘He’s Just Different Now’
Tom plays his trumpet for an Easter sunrise service, c. 2006. Three snapshots. Three brief glimpses over the past week that, like the rest of my snapshots, help show you what life is like for a family living with dementia. Although Tom is the one LWD, in some ways, all those who interact with him are LWD as well. And that’s especially true for me as his care partner (for more on this term, see here). FRIDAY AFTERNOON: GRANDPARENTS’ DAY We took off in the middle of the day to visit our grandson’s school (he just started 4K) for Grandparents’ Day. Pre-dementia, this would have been an easy and enjoyable trip. With dementia, it was enjoyable and stressful, including: — Leaving later than I planned because no matter how early I get Tom started, it seems he needs more time. — Arriving to a crowded parking lot and ignoring Tom’s demand that I double-park. Because of his leg and back pain, I would like to have dropped him off at the door, but I knew he might not remember to wait for me. We had to park across a two-lane highway and walk down a small hill to the school. — Watching Tom make a beeline for the cookie table as soon as we entered the cafeteria (first Grandparents’ Day stop). All the other grandparents were waiting in line, so it felt a little awkward, but it didn’t cause a problem. — Because God providentially brought our grandson’s other grandparents there at the same time, we entered his classroom together. Lincoln’s delighted “Nana and Papa! Grandma and Grandpa!” made everything worthwhile for all of us. — Following Lincoln through two crowded hallways so he could show us the STEM room. With a very active almost five-year-old and Grandpa on a walker, this was challenging enough, but it became even more so when Tom left for the restroom as soon as we arrived. Somehow, I was able to corral Tom, have Lincoln escort us, and return to the STEM room and then his classroom with no mishaps beyond my own elevated heart rate. — Returning to the classroom to learn that his teacher and his other grandparents had been concerned about our long absence. I found myself apologizing for a situation I couldn’t have controlled, and I thought: This is who he is now. He can’t plan ahead, so I need to learn to expect the unexpected. I also need to adjust the things we do together—or ask for more help along the way. He’s still Tom; he’s just different now. And it’s OK. WEDNESDAY EVENING: Tom has started helping with a children’s choir at our church. This came at his initiative; he has led many similar choirs over the years. Because music is so important to him, I thought it might be a good outlet and a way to give him another significant task. But it hasn’t turned out the way I’d hoped. And evenings can be a challenge for those LWD. During the practice time, I stay in the background, allowing him to lead alongside the children’s minister. So far, he’s more passive than active, watching and listening to the kids but not even trying to direct. He licks his lips constantly as he stares down at the music. The first night, he was...
read moreSnapshots of Dementia: 1 Corinthians 13 for Dementia Caregivers
(Photo by Fadi Xd on Unsplash) Note: My favorite (and only) niece was married this past weekend in a lovely ceremony that included a reading from 1 Corinthians 13. Thinking back on our wedding, where that same passage was read, moved me to write the following paraphrase specifically for caregivers of those living with dementia (“person LWD” in the paraphrase below). If I know all about dementia and can discuss my person LWD’s situation, but do not have love, I become a voice my person LWD would rather not hear. If I’ve done all sorts of research and understand what my person LWD and I are facing, and if I have faith to believe God can change it all, but do not have love, it matters not. And if I make all sorts of sacrifices, changing my work, adjusting my priorities, and rearranging my schedule on behalf of my person LWD, but do not have love, I haven’t helped anyone in any way. Love is patient when my person LWD forgets what I’ve said only moments before. Love is kind when my person LWD does something that will cause me extra work. Love is not jealous of the extra attention my person LWD receives from family or friends. Love does not brag about what a great job I’m doing as a caregiver; instead, love recognizes and affirms both my personal imperfections and my prayerful dependence on God. Love does not speak to the person LWD in private in ways it would not want known in public; it does not manipulate situations toward its own selfish outcome; it stays calm when the person LWD becomes agitated; it does not keep a mental list of how much it has sacrificed and how many times it has served. Love does not rejoice when others do things it considers wrong or inappropriate in relating to the person LWD; instead, it takes delight when more people appreciate the person LWD and want to build a relationship with that person. Love preserves the dignity of the person LWD; it never stops believing and hoping for the best while enduring even the worst of situations. Love never fails the person LWD. After all, any special insights and learning about dementia will one day disappear, as will the distinctions between those LWD and those not. Like the person LWD, we have only a partial understanding of the mystery that is the mind. But one day, all of our earthly concerns will fall away, and God will restore everything lost or broken. Long ago, my person LWD set aside their childish ways. But today, more and more, they are speaking, thinking, and reasoning like a child. Today; I understand only a tiny part of what my person LWD is experiencing; one day, I will have full understanding—and so will they. So many elements are fading from my person LWD’s life; faith, hope, and love remain; these three. Yet in every situation we encounter—past, present, and future—the greatest is love. —1 Corinthians 13:1-12, author’s paraphrase for those caring for someone...
read moreSnapshots of Dementia: Control Freak
(Wikimedia Commons) I remember the day when I knew I had to make a change in my parenting style. I don’t know that I heard an audible voice, but as I moved from the pantry to the table to count out the animal crackers for my children, God spoke: Stop trying to control everything. I’m not sure what I was afraid would happen if I didn’t count out the treats—that the kids would eat too many? That we’d run out too quickly?—but that day, I stopped. I poured the animal crackers into their little bowls (or onto their little napkins; I honestly don’t remember). Maybe one bowl had more than the other. Maybe it didn’t. But from that moment on, I stopped counting. And controlling. God’s animal cracker instruction served me well as my children matured, because throughout that process, I could control less and less: Their rate of growth. Their emotions. Their likes and dislikes. And ultimately, their choices about their lives. The realization that I could control little and shouldn’t control much saved our entire family a lot of stress. I learned to, as a friend puts it, go with the flow of the Holy Spirit. And although our family remained imperfect, I believe we were all much healthier and happier as a result. So tonight, when Tom once again went to bed at 9 p.m., exhausted from trying to function with huge gaps in his thinking, I found myself cleaning, just as I sometimes did when my kids were small and he was out on pastoral visits. For a busy woman, there’s something near-magical about a quiet house with no dishes in the sink, no mess on the counter, and no crumbs on the floor. But then I realized the source of my satisfaction: control. In our dementia journey, I have little control over lots of things. I can’t control: — How many times Tom will interrupt my work to ask for help with his word games; tell me meandering stories about his online golf game; or have me find his glasses, coffee mug, or remote. — How long he’ll use a walker or if that walker will someday become a wheelchair. — If he’ll get to play with our coming grandchildren as he has with Lincoln. — If he’ll remember how to make his coffee tomorrow (he’s forgotten a couple of times in the last few weeks). — If he’ll make it through a full church service this weekend (we’ve had to leave early the last two Sundays). — How long he’ll be able to take his own shower and dress himself, both of which he does with increasingly less skill. — If his words will continue to slow down until he loses them completely. — If he’ll remain at home always or need more care than I can someday supply. — If he’ll always remember our children. — If he’ll always remember me. I can’t control any of those things or a hundred more that cross my mind nearly every day. And so I clean. And think. And pray. And as I spend another hour or two alone before I, too, go to bed, I realize again that it’s not wrong to take control over these small areas any more than...
read moreSnapshots of Dementia: Choose Your Battles
(Photo by syklimkin on Unsplash) Choose your battles. It’s a familiar parenting principle—and one that works well for many aspects of life. Sometimes it takes a slight twist: Don’t sweat the small stuff. Look at the big picture. Don’t miss the forest for the trees. But however we say it, we mean to avoid turning small issues into big ones, which often happens when we argue or fuss. I’m not much of an arguer (Read: If there were an anti-confrontation vaccine, I’d be first in line.) But there was a time earlier in Tom’s dementia journey that, for some reason, I found it important to let him know when he was doing something I considered wrong or inappropriate. Part of that reason was that he had not yet been diagnosed. Although I suspected problems over a period of years, his first neurologist as well as a neuropsychologist told me he was fine. So when he did something that upset me or had odd, unusual behavior, I talked to him. Sometimes I corrected him. Sometimes I told him he was wrong. In reality, since he couldn’t control most of his actions or impulses, I was the one who was wrong. I thought my words would help Tom make some different decisions about what he said and did, but of course he couldn’t think logically anymore even if he remembered my comments. Today, armed with a new knowledge set as well as his dementia diagnosis, I approach these situations much differently. BEHAVIOR: Tom doesn’t answer me when I ask him a direct question. THEN: “When someone asks you a question, you should respond,” I remind him. “It’s how people know you’re listening to what they say.” NOW: I repeat my question after a few minutes or drop it altogether. Concentrating takes so much cognitive effort that he can’t focus on more than one thing. He genuinely does not hear me. And these days, he is less and less able to process enough information to give a response. I didn’t understand that then, but I do now. BEHAVIOR: Tom flirts with the female grocery store clerk, a practice I’ve asked him to stop. THEN: I don’t say anything to him at the store, but afterward, I tell him he has hurt me. I also spend time grieving over the state of my marriage. NOW: I either use the self-checkout line and let him “help” me with the groceries (our bags contain some rather interesting combinations) so we generally avoid such encounters. If we go through a regular line, I try to do most of the talking. If flirting happens, I ignore it (although if it ever became inappropriate, I would shut it down and explain to the clerk about dementia). BEHAVIOR: Although he can no longer drive, Tom acts as though he’s still in charge of our car, telling me where to stop or turn, gesturing (not in anger) to other drivers, and obsessing about our miles per gallon. THEN: Even when you know your backseat driver has dementia, this can be frustrating. I don’t argue with Tom, but I do ask him to stop acting as though he were the driver. “I’ve got it,” I say. P.S. That doesn’t work. NOW: I ignore his backseat driving as much as possible. He can’t drive because...
read moreSnapshots of Dementia: ‘I Can’t Care’
Photo Credit: Peter Conrad, Unsplash Although I’ve written about many painful parts of our dementia journey as well as some positive ones, I want to discuss a primary dementia symptom/sign that I’ve mentioned only in passing. If I had understood how big a role it plays in many types of dementia, I would have pushed for a diagnosis sooner and harder than I did. This known-but-unrecognized symptom? Apathy. If I had known about this close connection earlier, I would have realized that many of the following were not just abnormal, often hurtful actions but signs of something dangerous happening in Tom’s brain. All of these became part of our lives at least two years before Tom was officially diagnosed with dementia in the fall of 2019. — Withdrawal from friends: Always the life of the party who would keep talking to people long after I was worn out, Tom now waited for others to take the lead in group settings and often wanted to leave early. — Lost celebrations: He did less and less, sometimes nothing at all, to recognize birthdays, anniversaries, or other special days—a big change from the person who would find the most random of reasons to celebrate. — Lack of compassion: Previously an expressive personality, Tom displayed a flat affect/expressionless face even when he knew he had hurt someone (usually me) deeply. Prior to his diagnosis, we met with marriage counselors for nearly a year. At one point, they suspended our sessions because of this type of behavior and the fact that, even when they called him out on it, nothing changed. — Withdrawal from family: For a few years, Tom refused to travel with me to visit my widowed mother, saying he couldn’t take time off work. Later, he refused to attend a baby shower for our expected first grandchild for the same reason. Later, he came to see our newborn grandson for the first time only when I insisted he make the trip. — Lack of interest in his health: Tom stopped seeing the dentist several years before diagnosis and only went to the doctor when I insisted he go. He never seemed interested in what we were finding (or not finding) out about his potential dementia. It almost seemed as though this were all my problem, not his—which is what he told the neurologist who diagnosed him. Tom’s apathy showed up in other ways, but these are some of the bigger areas I noticed. In this video, dementia expert Teepa Snow explains some of the reasons behind the apathy associated with vascular and other types of dementia, including the frontotemporal variant Tom has. She says it’s not that the person with dementia doesn’t care anymore—it’s that they can’t care. The part of their brain that allows them to care about things doesn’t work anymore. In Tom’s case, his apathy now shows up in areas such as: — Clothing: He’s never had much interest in fashion, but he would now wear the same sleep shorts and undershirt all day, every day if I didn’t encourage him to get dressed. — Personal Hygiene: He often goes a few days without shaving, something he rarely missed in the past, and if I don’t urge him to shower, he won’t. — Activities: Some days, even activities he...
read moreSnapshots of Dementia: Significant Tasks
Tom singing at a nursing home, July 2022 A big part of my writing life has come through my relationship with Dr. Walker Moore of Back 40 Ministries. He and I have collaborated on three books and worked together in both his former and his current ministry as well as on the mission field. I’ve also edited his weekly column in the Oklahoma Baptist Messenger for a number of years, and we’ve shared in other publishing projects as well. One of my favorite teachings in our book Rite of Passage Parenting and its companion workbook is the concept of a significant task: a special assignment that demonstrates an individual’s worth to the people who are important to them. For a four-year-old, a significant task might be emptying the wastebaskets or helping sort laundry. For a fifteen-year-old, a significant task might be changing the oil in the car or taking responsibility for a part of the family budget. Those who don’t have significant tasks often look for significance elsewhere—often in inappropriate ways and places. I realized not long after Tom’s official diagnosis that one of the wounds for people living with dementia comes from the loss of their significant tasks. Near the end of 2018, Tom experienced the loss of his worship pastor job followed by the loss of the ability to hold a job at all. Within a few months, our family also asked him to stop driving—another loss of a significant task. And before all this, when he secretly gave away thousands of dollars to online scammers, I took over our finances and removed yet another significant task. I didn’t want to manage everything, and my personality is by no means controlling. But Tom’s dementia has meant I have no choice but to be in charge of our significant tasks. So how can he still know he has value and purpose? My solution has been to let Tom be as responsible as he is able as long as he is able. These are his primary significant tasks: — Coffee Service: Tom loves coffee; I do not, so he’s almost always made the coffee in our home. Before we sold our Florida house, our son had to repair a warped kitchen drawer because Tom had forgotten to put the carafe under the coffeemaker so many times. A few years ago, our wise children gave him a coffeemaker that dispenses only a cup at a time. Tom still has frequent spills (yesterday’s soaked two bath towels plus), and I often find him reading the instruction sheet for the coffeemaker over and over. I’ve started helping him more, but I want him to keep this task as long as he can because it means so much to him. — Water Delivery: I don’t drink coffee, but I do drink at least one large travel mug of hot water or hot tea every day. When we moved to South Carolina and I went back to working from home, I asked Tom if he would bring the water to me at my desk. He can still perform this task, although he almost always forgets for a few hours. I try to let him remember on his own and always thank him. If he keeps having trouble with coffee spills, this task will have to change as well. — Trash and Recycling: Tom still wheels our trash to...
read moreSnapshots of Dementia: Prone to Wander
Facebook/Project Lifesaver “You never know. I might get out.” This phrase, or some variation of it, comes up every so often in conversations with Tom. Although he struggles with both memory and language, his sense of humor remains intact. He thinks the tracking ankle bracelet he wears is unnecessary, but he complies with it because a. he likes the deputy who helped us get it, and b. I keep reminding him he wears it for my peace of mind. The peace of mind part is all too real. I wrote here about how I had to rush home from work one hot Florida day because he had (against a friend’s counsel) left home to walk to a mall about four miles away for an errand that could easily have waited until someone could drive him. Ultimately, I had to get the police involved in finding him. Although that story had a happy ending, I’ve never forgotten how it felt to drive the neighborhoods, praying and crying as I searched for him. Not long after we moved to South Carolina, I heard from one of the Facebook dementia support groups I belong to about Project Lifesaver (from its website): Project Lifesaver is the premier search and rescue program operated internationally by public safety agencies, and is strategically designed for “at risk” individuals who are prone to the life-threatening behavior of wandering. The primary mission of Project Lifesaver is to provide timely response to save lives and reduce potential injury for adults and children with the propensity to wander due to a cognitive condition. I also learned through another connection that Project Lifesaver was available in our county. By that time, we had had two more incidents of Tom “wandering,” both during the week (April 2020) a tornado hit our area. Our home had no damage, but the storm knocked out our power for almost a week. That very first day, our routine was much different than normal as we checked on neighbors and waited on the power to return. And also on that very first day, Tom took off without telling me where he was going. Fortunately, I saw him leave and was able to bring him back without incident. But later that day, we moved to our daughter and her family’s home because they still had power. During the week we were there, Tom took off on another walk, destination unknown. This time, he refused to come back when our daughter called to him. She had to jump in a friend’s truck and chase him down—another scary time. As soon as I learned that our county had Project Lifesaver, I contacted our local sheriff’s office, which manages the project. The ankle GPS units are issued via grants, and none was available. But within only two months, the deputy in charge contacted me to see if we could come in to have Tom fitted. That’s where the phrase “I might get out” started. Somehow during our conversation with the deputy, she spoke of people with dementia wandering, or “getting out.” Tom found that highly amusing, not realizing that he had, in fact, “gotten out” more than once. And although he forgets many things, he has held onto that phrase ever since. And he’s also gotten out. Every once in a while, usually...
read moreSnapshots of Dementia: You Didn’t Know Him
Tom ministering in Mexico. You didn’t know him when he prepared a set of Scripture verses for us to memorize together. You know him now, when he may not remember what you told him two minutes ago. You didn’t know him when his anointed trumpet playing moved people to worship—and even to tears. You know him now, when he rarely picks up his horn. You didn’t know him when he gave me a “book of the month club” that he kept up for several years. You know him now, when he doesn’t give any gifts without assistance. You didn’t know him when he labored over his sermons to make sure they were both biblical and practical. You know him now, when he has trouble paying attention in church or Sunday school. You didn’t know him when he loved to travel and meet new people. You know him now, when he prefers his home and recliner to anywhere else. You didn’t know him when he tried to spend special time with each of our children. You know him now, when I can’t always interest him in talking to them on the phone. You didn’t know him when he had such a sharp sense of humor that people said he should be a comedian. You know him now, when he repeats the same jokes and stories multiple times. You didn’t know him when he managed all our family finances. You know him now, when the government won’t allow him to receive his own Social Security checks. You didn’t know him when he planned elaborate dates and celebrated events such as our 3,000-day anniversary (which he figured out pre-internet). You know him now, when he rarely thinks of one day as different than another. You didn’t know him when he could lead a choir with musical expertise and spiritual passion. You know him now, when he often struggles to follow the music as he sings. You didn’t know him when he loved to drive. You know him now, when he has no license and hasn’t driven for more than three years. You didn’t know him when he insisted all the senior adults go first at our church potlucks. You know him now, when he scoops up handfuls of macaroni and cheese at the church fellowship because he can’t find the serving spoon. You didn’t know him when he was fully himself. You know him now, when the thief we call dementia has stolen so much. The person my husband is today is not the person he was, and yes, that makes me sad. But the person he is today is still someone who cares about God and others. Someone who still encourages people and loves to make them smile. And even if those things weren’t true, he would still be someone worthy of love. Someone worthy of respect. Someone who matters—because life matters. And even though his life looks much different now than it did when we married almost thirty-nine years ago, or five years ago, or even last year, it is one of profound meaning and inestimable value. I believe life matters, but not only at its beginning. If we truly believe in life, we believe that an individual’s value is in no way diminished by that individual’s physical or intellectual abilities, capacity, purpose, or potential. All the...
read moreSnapshots of Dementia: Not My Problem?
Photograph © Dennis Minty, 2022. When my mom and I took our recent cruise, I left my caregiving responsibilities behind—but as I wrote last week, they didn’t leave me. And guess what? Dementia didn’t leave me either—even when it wasn’t my problem. On our first expedition day when we left the ship to visit Sable Island, Mom decided to stay behind. We left the ship according to color groups, so when the leaders called ours, I headed to the mud room—where we prepared to disembark—without her. As I pulled on my waterproof pants, rubber boots, and other equipment, I noticed a woman I’d seen when Mom and I were having our boots sized. We’d introduced ourselves, and I remembered her name. Today, she was visibly upset. “I don’t have a backpack,” she said. “My shoes will get all wet.” On the trip necessities list was a backpack (and dry bag to hold it) to carry hiking shoes, phones, and anything else we needed for off-ship excursions. I’d already planned to carry Mom’s equipment in my bag. “I can take your shoes,” I told the woman. “I have extra room.” She seemed overjoyed. “Oh, thank you! Thank you so much!” she told me as I stuffed her shoes into my pack. She disappeared after that, but I knew I’d find her on the island. I didn’t think she’d attempt a hike in her rubber boots. For the next few minutes, I finished preparing, then followed the procedure we’d learned for safely seating ourselves on the zodiac. Despite some fog, we had a fairly smooth ride and landed on the island with the help of our “spinners,” who turned the zodiac and pulled it onto the beach. Next, I headed for the area where we could change into our hiking boots. I didn’t have a hard time finding my new friend—not because she was looking for me, but because she was looking for her shoes. “I can’t find my hiking shoes,” I heard her tell someone else. “I don’t know what happened to them!” “I have your shoes!” I said, pulling them out of my pack. Once again, she was overjoyed—momentarily. She didn’t say, “Oh, that’s right!” or “Of course!” She just accepted the shoes and moved on. And I wondered. From then on, I kept noticing this woman (I’ll call her L). Although L had an extensive vocabulary and could carry on an interesting conversation, every time I encountered her, she seemed a step behind. Once, she showed up with our color group on a tour segment—but she belonged in another. I saw others shaking their heads at her evident confusion. And I wondered. Another day, I was waiting in the ship’s lobby when L appeared—agitated and anxious about an off-ship excursion. Another woman explained what she would need, and L strode happily off to retrieve it. After she left, the other woman told me about multiple problems that had occurred because of L’s confusion. She seemed upset that another woman, L’s longtime friend, had in effect become her caregiver during the trip. And I wondered. I knew God must be putting something together when, the next day, I ended up alone with L’s longtime friend. In just a few questions, I determined that no, this was not typical...
read moreSnapshots of Dementia: The Rest Is History
Mom (R) and I aboard the zodiac (small rubber boat used for off-ship excursions). I mentioned in my last post that I had the privilege of having some time away, and I’ve also written on social media about my amazing trip with my mom (her ninetieth birthday present from our family). This was a bucket-list item for her, a small-boat cruise off the Atlantic provinces of Canada, but it ended up being the trip of a lifetime for us both! Mom and I share many of the same interests, including a continuing love of learning. This trip was perfect for us because not only did we get to see lots of amazing sites—including Sable Island, a coveted destination spot that boasts its own herd of 500-plus wild horses—but Adventure Canada brought biologists, anthropologists, naturalists, and more along to help us understand and appreciate everything we saw. Mom and I will be forever grateful for the many growth opportunities as well as the wonderful new friends we met. During our trip, I also discovered some things about myself and my caregiving situation. Here are five things I learned during my time away. 1. I needed a break: The first few days of our trip, I slept. A lot—ten to twelve hours at night with some daytime naps as well. I was amazed at both how tired I was and how good it felt to get enough rest! It also took me those first few days to realize that I’ve been living without adequate rest. I plan to correct that because I enjoy the way it feels to have sleep, and I know it is much better for my life and my health in general. 2. Caregiving carries with it a unique level of stress. Yes, this is closely tied to point 1. But wasn’t I also a caregiver on my trip? You might think so, but my mom is amazingly sharp, with only mild, age-related cognitive decline. I did have to open the heavy doors, carry our bags, and watch out for her on stairways and hikes, but I did not have to make all the decisions, ensure her safety every time we went anywhere, and carry a private concern that she might say or do something inappropriate. Those are all part of what makes even a simple trip to the grocery store with Tom an increasing challenge. 3. I now view the world through a caregiving lens. I tried hard not to talk about Tom or caregiving all the time (although I’m not sure my mom would say I succeeded). I do know that he was often in my thoughts, and I realized for the first time that I now relate to much of the world in terms of my caregiving responsibilities. I didn’t tell everyone I met about Tom’s dementia, but whenever I spoke to someone at any length, it seemed to come up. One of the experts on our trip works for Birdlife International, and on a zodiac ride I shared with him, I found myself telling him the story of how much Tom, as a person living with dementia, enjoys watching the birds who visit our feeders—and we were only together for a few minutes! 4. I’m not irreplaceable. Our daughter Melanie, who lives in Indiana, came for nearly three...
read moreSnapshots of Dementia: My Favorite Things
Tom’s walk-in turtle pen Some of my posts carry a lot of emotional weight, last week’s being a good example. Since living with dementia itself carries a lot of emotional weight, in order to present accurate snapshots, I do my best to let you see what I see and even feel what I feel. But sometimes, what I feel is not sadness but love and light. Back in our child-rearing years, God sometimes allowed me to step outside of the chaos and catch a glimpse of the beauty. He does that with dementia too. So, lest you think we’re living in constant heartbreak, please know that we also have times of genuine joy. I find that joy when: — Our primary care physician speaks to Tom as a real person, laughs at his humor, and waits patiently for his responses. — Our four-year-old grandson can’t wait to go bowling with Grandpa. — Our young worship pastor shows respect for Tom’s musicianship as well as his sense of humor. — We spend the morning running errands, which will wear Tom out for the rest of the day, and he tells me, “This was the best day ever.” — Tom expresses amazement when I find something, usually his reading glasses or the TV remote, that he’s lost for the fourth time in an hour. — A friend texts us just to check on us and remind us how much we mean to her. — Our nearby children invite us to meet them for a spontaneous meal or other treat. — Our farther-away children call or video chat with us. — The staff of our local library gives every indication of helpfulness and no indication of annoyance when Tom gets confused during the checkout process. — Our senior pastor refers to him as “Pastor Tom.” — Tom finds delight in a simple meal because for him, simple is good. — A doctor or other medical staffer looks at the whole picture of his health rather than pulling out one specific element. — Tom blows a few notes on his trumpet or gives our son advice about how to play a particular song. — Our oldest daughter hand-picks two of her students to help her build a walk-in turtle pen so her dad will stay safe when caring for his beloved box turtles. — We visit a nursing home with our church’s senior adult choir, and Tom not only sings beautifully but speaks words of encouragement to every resident he meets. — I look forward to some time away, knowing our youngest daughter, with help from her siblings, will keep Tom both happy and healthy while I’m gone. (More about that in my next post.) If you’re a dementia care partner, what brings you joy? Share your thoughts in the comment section below or on social media. Our story matters—and so does...
read moreSnapshots of Dementia: Inside Edition
A recent photo of Tom in his recliner, one of his birthday gifts this year. Although I shared a guest post last week, most of the snapshots of dementia so far come from me. Today, I wanted you to hear from someone else—someone who’s been present throughout our dementia journey. That person is my husband of almost 39 years, who has been living with dementia for at least the past five years and probably much longer. As Tom’s symptoms progress, he has increasing trouble focusing on more than the simplest information. Always a creative who loved to share ideas and information, he used to say he didn’t think outside the box—he couldn’t even find it. Today, his cognitive box is small—and it shrinks a little more every day. I conducted the following “inside edition” interview one evening this week—not the best time for him because of the sundowning I mention in this post. Despite my editorial distaste for ellipses, I’ve used them here to indicate pauses—sometimes long ones. I consider this a true snapshot of dementia: Tom’s perspective in his own words, even when his answer doesn’t match my question. MP: So if you were going to tell someone what it’s like to have a young-onset dementia like this, what would you say? TP: It is just deceptive. One point, you can be clear-headed. . . and putting footstep after footstep, and then other times, you. . . it’s. . . You know that I. . . I try to. . . try to keep a good. . . attitude and. . . it’s frustrating to me that like, when I have sundowner’s, because it just. . . it’s just like Let’s Make a Deal. You open it and suddenly you’re just there. You can’t change your emotions. . . Your continued encouragement and taking care of me and setting up stuff for me. . . it’s so encouraging. Sometimes you have pulled me off the cliff … and I feel encouraged and loved and cared for. . . . I never in any of my dreams ever thought that this is where I would be now (tears). MP: What do you think is the hardest thing for you about having this disease? TP: One thing would be. . . there are times when I can walk, and. . . I try. . . I try to keep reading because I don’t want to be locked in on word games and my golf game [both games he plays on his iPad]. . . . There’s not very many times that it happens, but sometimes you are wanting to do something or wanting to go someplace. . . and I’m trying to. . . I always love going someplace with you, which is not to say that I don’t love being with you right now. . . . It’s almost just. . . like one day you wake up and you can walk 10,000 miles, 10,000 steps I mean, and then another day. . . . I would be scared to go any place without my walker. MP: You know, so far, we haven’t used your walker. {He’s had a walker for about three weeks but has so far avoided using it.] So are you saying you’d just stay at home...
read moreSnapshots of Dementia: Sunrise, Sunset, Sundowning
Photo by David Mullins on Unsplash As I’ve said before, Tom and I are the typical opposites who attract. We realized early on in our marriage that even our sleep patterns differed. I could remain alert late at night but took a while to feel like talking in the morning. He needed an earlier bedtime but arose, fully recharged, no matter how early the alarm clock rang. All that changed, however, with the arrival of our first child—and then our second ten months later. I’ve often said that mothers have to be both night owls and early birds. Once again, my parenting experience has served me well, as I now need alertness at many times of the day. That’s especially true because over the past several months, sundowning has played a more significant role in our lives. In case you haven’t heard of sundowning or sundown syndrome, it refers to a set of symptoms that typically occur as daylight begins to fade, generally in older adults with one or more forms of dementia. It can involve restlessness, agitation, irritability, confusion, and more—and it often makes going to bed and staying asleep a challenge. Tom has taken medication to help him sleep since we first began treating his dementia symptoms, so I suppose he’s shown sundowning behaviors for a while. Without the medication, he tends to wake up much more or becomes agitated, even violent, in his sleep. With the medication, he sleeps well—for the most part. As a person living with dementia, he also requires more sleep than he used to. The activities of daily living are much more difficult for him than in the past. His broken brain has to work harder to process simple conversations and ideas. If we have an outing or appointment during the day, he almost always comes home exhausted. He still loves interacting with people, but the mental challenge wears him out. That exhaustion was one of those dementia symptoms I noticed long before the doctors agreed with me that anything was wrong. The simplest tasks seemed to tire him, and he took naps whenever he had the opportunity—something he’d never done before. I wondered if he was aging prematurely, and in a way, I guess he was. If you look at photos of him now compared to even a few years ago, you can see the toll his disease has taken on his face. Of course, that’s nothing like the toll it has taken on his life. Tom’s sundowning means I can’t ask him questions late in the day and expect a coherent (or any) response. His tremors worsen, so he’s more likely to spill his food and drinks. For the past month or two, whether or not we have an outing, he often takes a late-afternoon or early-evening nap and is still ready for bed as early as 8 or 9 p.m. When he goes to bed this early, he may have a restless night, or he may sleep well. Trying to get him to take an earlier nap, as you can imagine, is about as effective as getting a cranky child to do the same. But there have been days when he’s taken naps morning, afternoon, and evening—and still gone to bed by 9 p.m. On some occasions, his sundowning results in agitation....
read moreSnapshots of Dementia: Tender Loving (Self-) Care
Roses from my garden, 2022 Friends and acquaintances often ask me how Tom is doing. The short answer is that there’s no short answer. The long answer? Well, I wrote about that here. If that question is a FAQ, this next phrase is an FMS: Frequently Made Statement. It comes in several different formats, but they all sound a lot like this: — “I hope you’re taking care of yourself.” — “Don’t forget to take care of yourself.” — “You know, you really need to take care of yourself.” You get the picture: I have friends and family members who want to make sure I’m not lost in the process of caring for Tom. I don’t think a lot about this topic until someone brings it up, but I do find ways of caring for myself. Just as the rest of our life looks very different now than it did only a few years ago, self-care looks different too. For one thing, I can rarely leave the house without Tom. For another, I’m the breadwinner rather than the freelancer who scheduled her work around family and other commitments. The COVID-19 pandemic hit not long after I began working from home and caring for Tom full time. For more than a year, we didn’t go out much at all. That and my God-given bent toward home and family shape my lifestyle even now. So, in no particular order, these are a few of the ways I practice self-care: — Exercise: I’ve been in the habit of walking at least three miles/day for many years. I try to do four or five miles a day now. Much of that happens inside the house because Tom’s leg pain means he doesn’t always feel like walking, but when we can, we still enjoy walking outside together. — Showers: After multiple mission trips to countries where water is a luxury, a shower remains a cherished gift. Right now, I can still shower while Tom rests in his recliner. Those few moments of peace, enhanced by my favorite bath products, provide simple but special self-care. — Worship: Worship feeds my soul and spirit more than anything else. When I attend choir practice, the songs stay in my heart all week and provide needed strength. If and when Tom can no longer attend church services, I plan to have someone else care for him so I can still go. Online church is a wonderful provision, but it doesn’t replace in-person connection. — Baking: Gone are the days of making 50 dozen cinnamon rolls over a three-day period to support our children’s mission trips. But I still love to bake, and that meshes well with Tom’s increasing desire for sweets. For both our sakes, I try to find a good balance. — Gardening: I’ve enjoyed adding roses, daylilies, and other plants to our yard over the time we’ve lived here. Working in the garden always brings me joy, and even if I run out for only a few minutes to water a plant or deadhead a rosebush, I return refreshed. — Feeding the Birds: A few months after we moved here, I bought one bird feeder. That one has now become six, two of which are attached to my office window. I never thought I...
read moreSnapshots of Dementia: That Time We Were Glad He Forgets
Photo by Valeriia Bugaiova on Unsplash Throughout our dementia journey, good times and challenging times have intertwined. God’s sovereign hand means even the darkest of circumstances can dawn bright enough to be a blessing. We also know that even the happy times carry a profound element of grief. This past winter, an unusual chain of events transpired that reminded me that even those times of forgetfulness and confusion play a part in the way God “causes all things to work together for good to those who love him and are called according to his purpose” (Rom. 8:28, NASB). We experienced this in the fall of last year, and it began with a physical fall—one that only happened because of Tom’s dementia. He and I had done some Saturday shopping at a local grocery store. I’d had reverse shoulder replacement surgery only weeks before and still had one arm in a sling. With my one good arm, I was loading the groceries into the back of our car, Tom by my side. As we finished, our grocery cart rolled down the store’s sloped parking lot, and a woman driving toward us honked her horn. I turned around, but it was already too late. Tom was running to retrieve the cart, both hands in the air, swinging his body from side to side. Despite his panic, there was no emergency; the cart wasn’t rolling fast, and we could have retrieved it. The car, a large SUV, wouldn’t be damaged by its impact. But a real emergency loomed. In my head, Tom had already fallen and I was calling 911. And then it happened. He fell flat-out, right in front of the oncoming car (mercifully stopped at this point). Within seconds, I was by his side. “Baby! Are you OK?” I said as he lay there, stunned. “I think I am,” he said as I helped him up. I told the driver that he was fine, and she drove on around us, no doubt wondering why he had run as he did to retrieve the cart. I didn’t wonder. I already knew that dementia had stolen Tom’s “safety” mode. When his fight-or-flight response kicks in, it’s strong and immediate. But I also knew he might not be fine. But since he hadn’t lost consciousness and had no obvious injuries, I took him home. By Monday, I called our primary care physician because his pain had increased, and I feared he had broken a rib. It was now Thanksgiving week, and she had no appointments, so her office sent us to an Urgent Care. An x-ray showed two broken ribs—and a large mass in his left lung with extending fingers to the lymph nodes. Once CT scan and two appointments (one with our own doctor and one with a pulmonologist) later, we were facing the strong possibility that Tom had lung cancer. I let our children know what the doctors had said and waited for the next appointment: a bronchoscopy and biopsy. The pulmonologist would sedate him lightly and explore his lungs with a lighted scope, taking biopsies so we would know exactly what was wrong. So why were we glad Tom didn’t remember and, probably, didn’t understand? Because throughout this ordeal, for only a few hours did he understand he might have cancer. Sometimes, he has moments...
read moreSnapshots of Dementia: Memory Matters
Photo by RoonzNL on Pixabay Although the frontal-lobe aspect of Tom’s dementia means we noticed devastating behavioral changes, his memory loss has also been a consistent sign and symptom. Throughout our journey, I’ve heard comments such as, “Oh, I forget things all the time!” or “I do that too—maybe he’s not as bad as you think!” While yes, we all forget things, there is a definite difference between forgetfulness associated with normal aging and forgetfulness associated with dementia. I won’t go into those details here, but you’ll find a good explanation at this link. In short, experts often use the term “memory loss that disrupts daily life” to distinguish it from more normal, age-related memory loss. I’ll give you a few examples from various points in Tom’s journey that I hope will illustrate why memory matters and how debilitating it can be. Work: While Tom was still employed as a minister of music, he had increasing trouble keeping track of the details needed to serve a midsize congregation (around 500 in attendance total at three different services). The last year or two, when he led choir rehearsal, he invariably left one or two songs out of the audio file he had prepared in advance. After he lost his job and I spoke with our former senior pastor (who had retired the year before), I learned that often, he and Tom would have a discussion that Tom didn’t recall even a few days later. During this time, he also struggled to use his in-ear headphones and fumbled with his mic nearly every week; he also forgot preplanned details of the services. Home: Long before diagnosis, we had to install special hinges on our front door to close it after Tom left it wide open more than once when he left for work. Nowadays, his memory has declined enough that he leaves other doors open on a regular basis: cabinets, dishwasher, refrigerator, freezer—I often think about how short his memory must be if he can’t remember to close a door he has opened only seconds before. As you can imagine, he loses and has lost various items for years—I’ve sometimes wished I could have all the time back that I’ve spent hunting for them! We do use a Tile tracker and connected app on the most essential items, but it’s amazing how quickly he can lose the remote, his phone, his reading glasses, his coffee mug, or whatever object was last in his hand. Outings: Memory loss makes it increasingly difficult for Tom to navigate places he doesn’t know well. When we go to a store and he needs to use the restroom, I stand near the door, or he won’t find his way back to me. He hasn’t driven for nearly three years now, but when he—who, unlike me, had always excelled at directions—couldn’t find even familiar places, I knew something was wrong. For right now, we still sing in our church choir, but he invariably gets confused about how to get from the choir room to the platform, and I try to make sure one of the other men helps him navigate. Relationships: Memory loss affects his relationships as well, and this goes beyond the normal not remembering someone’s name that we all experience at times. He does remember some people, but...
read moreSnapshots of Dementia: Roller Coaster Ride
Photo by Justin on Unsplash Twists. Turns. Slow, then fast. Up, up, up—then plunging down. And sometimes, what seems like a complete reversal. That describes not only a roller coaster ride but our journey to and through diagnoses (intentional plural). In this post from a few weeks ago, I shared how after a long wait, Tom was finally approved for disability payments through the Social Security Administration. I no longer had to jump through hoop after hoop to get doctors to agree that something was wrong with him and/or agree on a diagnosis, which had previously wavered between frontotemporal degeneration, behavioral variant, and young-onset Alzheimer’s Disease (“young” onset means symptoms develop before age 65, and Tom had symptoms well before age 60, which is when I finally convinced him to see a neurologist). As it turns out, we weren’t done with the diagnosis process after all. As I also mentioned in that post, we had one unsatisfactory visit to a neurologist in our new home state of South Carolina (where we moved in late 2019; we had seen a total of four neurologists in Florida). Once the perceived urgency of diagnosis was over, I didn’t want to go back to that doctor. I took the advice of a local friend and called the Brain Health Center at Emory University in Atlanta. We had tried to get Tom accepted there once before, but at the time, they wouldn’t take patients who lived more than an hour from the hospital (we live two hours away). Both the pandemic and the fact that Tom now qualified for Medicare helped us. When I called in the spring of 2021, the screener said she would call me back “in a day or two” if he qualified. I got a call back that same afternoon. A few weeks later, we met with Tom’s new neurologist for the first time—via Zoom as we sat parked outside a restaurant in Georgia (we had to be physically in the state because of medical licensing requirements). They had no in-person appointments, but I filled out multiple questionnaires ahead of time. The neurologist listened to both of us (although Tom stopped participating early on), asked insightful questions, and wanted to hear various details of Tom’s health. I mentioned that although many of his behaviors/symptoms were consistent with FTD, his early memory problems seemed to point more toward Alzheimer’s, and he had received both diagnoses. To firm up the diagnosis, this neurologist recommended a lumbar puncture and an MRI (his third since 2017). We had declined a LP a few years prior, concerned about putting Tom through a stressful procedure, but this time, I said yes. Since I had gone to the trouble of taking him out of state to a top-rated brain clinic, I felt I should follow the neurologist’s recommendations, and he felt these tests were necessary to provide the best treatment for Tom going forward. We couldn’t get an appointment till November, but he could have both procedures done the same day. What I didn’t know in June was that I would end up having shoulder surgery in early November, so our oldest daughter drove Tom to his appointments and accompanied him to both the tests. In her characteristic style, she also made sure he had a fun day that included...
read moreSnapshots of Dementia: 5 Ways Parenting Prepared Me for Caregiving
Pieper Family, 2003 “It must be so hard.” “I know you didn’t expect this.” “No one thinks about this when they say their wedding vows.” I’ve heard all the above comments my status as the spouse of a person living with dementia. All are true. But, like almost any other statement someone might make, none reflects the full picture. Yes, it is hard. No, I didn’t expect it. And no, I didn’t think about this particular situation when I said my wedding vows—although I did, and do, believe “for better or worse” means exactly that. Of course, my faith also means I believe God knew Tom and I would one day find ourselves here. Not only that, but I also believe He prepared me for the role of care partner long before I ever officially (and, before that, unofficially) accepted that assignment. One of the ways He did this was by allowing me the privilege of parenting five children. Parenting shaped my life and my character in significant ways, many of which made me the person I am today. Of course, I am neither a perfect parent nor a perfect caregiver, and I hope my writings in this blog and elsewhere never imply that. Instead, I consider myself a grateful parent and caregiver who knows God has called her to this specific assignment at this specific time and done what He always does when He gives an assignment: prepared me to accept it and equipped me to pursue it. Here are five ways I believe parenting prepared me for my current role: 1) Parenting taught me patience. Parents either learn patience or make themselves and their children crazy. Of course, patience is also a fruit of the Spirit, so I have some supernatural assistance in this area. Whether in dealing with Tom’s obsessive behavior, repeating an answer to a question he has already asked multiple times, or following behind him to close doors/pick up dishes/retrieve misplaced items, I need lots of patience. Every day. 2) Parenting made me flexible. My experience both as a parent and as a sometime-missionary taught me to go with the flow. When I first took a 9-5 job after many years at home, one of my coworkers told me I was the most laid-back person he had ever met. But that didn’t always describe me. Once again, God used my parenting experience to help me realize things don’t always go as anticipated and that getting upset helps no one. When Tom takes longer than I expected to get for an activity even when I’ve allowed what I thought was extra time, or when his dementia means our plans must change on short notice, this quality has served me well. 3) Parenting helped me become a better listener. Almost every mom will tell you she hears what her kids say and learns to hear what they don’t. As children grow, they tend to tell their parents less. A wise mother learns to interpret attitudes behind actions, capitalize on what are often rare moments of openness, and catch the unspoken behind the overt. As Tom moves further in his dementia journey, his language skills are declining. He says less, and what he does say may come out halting or confused. I’ve learned to discern (most of the time) when his statements are...
read moreSnapshots of Dementia: Two Is the Loneliest Number (and Other Reasons I Cry)
Photo by Xianyu hao, Unsplash I am a person of tears. I cry when I’m sad. I cry when I’m happy. I cry when I worship. I cry—you get the picture. My children remember me not as the mom who screamed when they were disobedient but as the mom who (you guessed it) cried. I’ve written before about these tears here and how, in Tom’s (more and more rare) moments of awareness of his condition, sometimes, we cry. As far as I can tell, I feel things more deeply than many people. I believe this quality makes me a better intercessor and a better writer, but it also means that, as the wife of a man living with dementia, I cry. Why do I cry? Not because of the pain of the past, the years when doctors kept saying Tom was fine but his behavior showed us he wasn’t. Not because of the responsibility. Yes, it still feels like a weight—being in charge of everything about our lives together, from small to big decisions, tasks, schedules, and everything in between—but God has given me what I need, and I’m consistently amazed at His provision. Not because of the diagnosis. Knowing Tom has what I consider a terrible disease makes me sad, but we waited so long to receive medical affirmation of our suspicions that when it came, I felt more relief than sadness. Not because of lost jobs. I did cry—a lot—when Tom had to leave his final worship pastor position. We loved our church and the people there. But Tom was in such a bad place emotionally/spiritually/and of course cognitively at that time that I knew something had to shift. So although the tears came, I also realized it was time, probably past time, for him to go. So why do I cry? Because of our children. Every mother will tell you she’d rather hurt a thousand times herself than see her child hurt once. All our children are grown now, but their father’s disease still wounds them. We all hate the way dementia is stealing him from us. And I know it gives them additional concerns for the future, all of which I wish I could remove but none of which I can. Because of our grandson. As I wrote about here, Lincoln and his love for Grandpa have taught me much about genuine love. Lincoln doesn’t mind that Grandpa gets mixed up easily, makes awkward comments, or doesn’t remember what someone told him only a few minutes earlier. But knowing that this little boy will continue to grow, change, and progress while Grandpa grows, changes, and regresses? That makes my heart hurt and my tears flow. For Grandpa—and for a little boy who has never known him healthy and whole. Because two is the loneliest number (when one has dementia). I still talk to Tom as though he can understand everything I say. In reality, he needs information in small bites, and may not remember it even then. I still lean my head on his, hold his hand, and give him hugs and kisses. I still consult him on decisions even though in reality, he won’t offer input. But more and more, our relationship resembles that of a very large child and parent rather than that of...
read moreSnapshots of Dementia: It’s Complicated
Photo by TheDigitalArtist on Pixabay That brief phrase might be my best answer to the question I hear most often about my husband: How’s he doing? I doubt those who ask have time or desire to hear the long version of my response. So “it’s complicated” works well. Before I had the privilege of carrying a child, I thought pregnancy meant you gained weight, your abdomen grew larger, and in nine months, you had a baby. I had no idea that so many areas of my body, from hair to fingernails to feet, would change as I journeyed through those months. That’s how dementia is. Before it struck our family, I pictured it as a primarily a memory problem. For Tom (but not for all people living with dementia) memory loss plays a big part, but dementia affects so much more than memory. The best way I can think of to explain “it’s complicated” is to compare how he was two years ago (just after we moved to our home in South Carolina) to now in several key areas. 2020 SPEECH: Has become increasingly halting. VISION: Poor depth perception. MEMORY: Remembers many people but not dates and events; needs daily reminders to take medication. DIET: Normal, some food and drink obsessions. Has lost his sense of smell, which has begun to affect his sense of taste; likes and dislikes are changing. HOUSEHOLD TASKS: Little initiative to help on his own but vacuums, mops with reminders, and does occasional other chores. FINANCES: Can no longer manage bank accounts or personal finances; still has a debit card and one credit card that I monitor. EMPLOYMENT: Retired after losing three successive jobs in late 2018/early 2019, all dementia-related but has no benefits. DRIVING: Our family asked him to give up driving in April 2019 after minor accidents plus observation of his driving; still wants to transfer his Florida driver’s license to South Carolina “just in case.” PERSONAL CARE: Normal except that he stopped going to the dentist a few years ago and needs treatment. BALANCE: Diagnosed with a balance problem in late 2019 and had a few weeks of physical therapy. SWALLOWING: No known issues; coughs (a lot) and chokes (sometimes). SLEEP: Normal; was acting out his dreams and had restless nights until one neurologist prescribed an antidepressant. INTERESTS: Decreasing; still engages with family with encouragement, enjoys church, music, movies, TV, reading, golf, and has obsession with an online golf game. Will often choose this game over engaging with family. A former professional trumpet player, he has not practiced consistently since May 2017. 2022 SPEECH: Much slower with frequent pauses, often gives up. VISION: Narrowing field, misses many objects. MEMORY: Remembers people but often forgets names; rarely knows what day it is; I now dispense all medication. DIET: Appetite control seems “broken,” can consume huge quantities or very little without seeming to notice. Obsessed with sweets, pepper, and very hot food. . HOUSEHOLD TASKS: Willing to help but rarely follows through; still helps when we work together. FINANCES: No longer has any bank or credit cards. I tried a children’s debit card with controls, but he lost it. EMPLOYMENT: The Social Security Administration declared him fully disabled in February 2021. DRIVING: No longer has a desire to drive but sometimes calls out...
read moreSnapshots of Dementia: Four Things I Learned in My Crash Course
Yours truly with our oldest daughter, one day post-crash Crash. That’s what happened to me in mid-May last year. No, it wasn’t a car accident. We were visiting our local daughter and her family, who all had brand-new bikes. Our then three-year-old grandson was out riding his bike along with his 15-year-old foster brother (if you missed H’s story, find it here). “Mom, you can take my bike if you want and ride with them,” my daughter offered. Never mind that I hadn’t been on a bike for years. I used to ride a unicycle, so a bike should be no problem, right? Never mind that I need to stay well for my husband’s sake. Bike riding helps keep people healthy, right? Never mind any of the second thoughts I’ve had since that eventful day. I dutifully donned my daughter’s helmet (for which I am still thanking God) and rode down their long driveway behind the boys. I won’t bore you with all of the details, but after a few successful rides up, back, and around the drive and cul-de-sac, I hit some gravel. The bike flew one way, and I flew the other: down. Cut to the emergency room, one stitch in my left eyelid, bandages over deep wounds in my elbow, bruises and swelling on my face, and a broken left humerus (upper arm bone). My daughter, who went with me, brought me home around midnight. Under the influence of pain meds, I lost consciousness at home early the next morning, hitting my forehead on a door and wedging myself inside the bathroom in the process. My new motto: Go big or go—back to the ER. Another visit there for my daughter and me, but thankfully no concussion or other major injuries (the giant hematoma waited a few days to pop up on my forehead). This began a long saga of doctor’s visits, physical therapy, and ultimately a reverse shoulder replacement and more physical therapy. Almost a year later, my arm/shoulder still isn’t 100 percent, but it’s much better. Tom didn’t crash. He didn’t even—thankfully—see the crash take place. But through this time, I learned a few lessons to add to my care partner knowledge, and I want to share them now. 1) “Big feelings” happen. This is true not just with our four-year-old grandson but for those living with dementia too. As soon as the ambulance left, Tom paced around our daughter’s backyard for an hour or so, crying. Seeing me leave in the ambulance upset him for days. His brain can’t process change well, and his amygdala, the part of the brain that handles emotions, was working overtime. Anyone would feel upset if their spouse had such a bad accident. For someone living with dementia, it’s terrifying. 2) I can’t do this alone. I am Tom’s primary care partner, which means I take care of his daily needs. He can still do a lot for himself, but I manage his life, make sure he eats, sleeps, showers, and so on, because without me, he might not do any of those things and wouldn’t do most of them well. I knew a day would come when I needed more than occasional help. I never realized it would come so soon. 3) Family matters. I don’t...
read moreSnapshots of Dementia: People Who Need People
Photo by Shirley Mitchell on Unsplash The truth of this Streisand classic has resounded in all our hearts over the past two years-plus. I knew the enforced time at home would prove more challenging for Tom (the original “E” in extrovert) than for me, the confirmed introvert. When the lockdown ended and we began getting out again, the joy I saw in his face and heard in his voice convinced me that we are indeed people who need people—and we would do our best to stay safe, but social. I’ve written about the blessings of family and how much we treasure time with our five children, our two sons-in-love, and our grandson. We thank God for them every day, and as I wrote in last week’s blog, we couldn’t have survived the pandemic (especially the adventures of 2021, which I’ll share in an upcoming post) without them. We’re also grateful for extended family across the country (you know who you are, and we love you). In addition to family, I am increasingly grateful for friends, who continue to give us the kinds of gifts we hold close in our hearts. Below, I list only a few: — The friend who sends Tom brief notes with links to cartoons that mesh with the quirky sense of humor they share. Tom rarely looks at email these days, but he does pay attention to those. Better yet, they make him smile. — The college friend of Tom’s who visited us early in the lockdown. He lived in Michigan, so when Tom told me he would be in the area for the weekend and wanted to stop by, I was sure this Reservist must have a military event. Only partway through his visit did I realize: There was no military event. Our friend had driven hours from home, spent the night in a motel, then driven several more hours that morning to reach us—only to drive all the way back to Michigan that same day. That’s more than friendship. That’s the sacrificial love of Jesus. — A missionary friend from several states away whose husband also has a frontal-lobe dementia. She and I had only met online until she went out of her way to stop by in person, also during the first phase of the lockdown. Even our quick side hug on my front porch meant a great deal to me—but as not as much as the prayers, hard questions, and support from someone whose path looks startlingly similar to my own. She brought me a sunflower, a lovely metaphor for the brave beauty that stands and shines through even the darkest of circumstances. — The college friend of Tom’s who messaged, then called early on when she learned of Tom’s diagnosis. She spoke with me—and then with him. Since then, she has called him periodically just to chat. I’m sure his conversation wanders, but he is at his best when he talks about old times. I so appreciate her willingness to fit Tom into her busy life. — Old friends from the churches we’ve served (in Texas, New Mexico, California, South Carolina, Florida) who stay in touch through various means, including this blog. Just knowing we have people who care about us—no matter what—means more than I can express. — New friends from our...
read moreSnapshots of Dementia: A Tale of Two Blessings
Photo by Colin Davis on Unsplash It was the best of times; it was the worst of times. It was the age of coronavirus; it was the epoch of pandemic. We had dementia before us; we had faith behind us. And through it all, we had a God who loved us and provided for our every need. We moved to our new home in the upstate of South Carolina in late November of 2019, right as the first echoes of COVID-19 sounded in far-off countries. We had only just started to settle in when the lockdown came, and especially because of Tom’s dementia, we exercised what many describe as “an abundance of caution.” “You don’t want him in the hospital without you,” our primary care doctor told me. “And that’s exactly what would happen.” So we watched church services online. We visited with faraway family members on the phone and online. Our local daughter and her husband did our grocery shopping. And for many months, we saw few people other than medical professionals—and family. We were then—and are now—so thankful for family. Yes, we could have quarantined from them as well—but without that at least weekly connection with our daughter, son-in-love, and preschool-age grandson, I’m not sure what would have happened. We needed those hugs, that laughter, that break from our increasingly quiet routine. Tom needed that. I needed that. As the lockdown wore on, a temporary family member joined us: a teenage foster grandson, a former student of our daughter’s. Arriving in November 2020, he would only live with her family for the rest of that school year. You might not think a fifteen-year-old special education student who had lived his entire life in South Carolina and a sixty-five-year-old man living with dementia who had traveled the world as a professional musician and pastor would have much in common. But in this case, you’d be wrong. We figured it out the first time “H” came to visit. Our daughter often taught from home, and sometimes H had school from home as well. But he didn’t always have to log in during the day, so he sometimes came to us instead. “I have to work, so he’ll be spending most of the day with Daddy,” I told our daughter the first time she asked if H could visit. “I know, Mom. They can just hang out.” And hang out they did. Turns out they had simple board games (Uno, Yahtzee, Sorry!, even Candyland) in common. H showed incredible patience when he had to remind Tom whose turn it was or when Tom argued about a roll of the die, which was often. He only chuckled when Tom got aggravated about losing, which was even more often. I had to step in once in a while with a word of correction—always for Tom, never for H. When Tom lost patience with board games (usually after an hour or two), they watched movies or old TV shows. Once again, H demonstrated amazing patience as Tom rolled out many of his old favorites, including those H had seen before. They laughed at the same lines, and if H failed to do so, Tom made sure he knew why he should have. And once again, H never complained. I soon realized this...
read moreSnapshots of Dementia: Not-So-Easy Money
Photo by Giorgio Trovato on Unsplash Regular (minus a lapse of nearly a year) readers of this blog may remember that Tom received a diagnosis of young-onset Alzheimer’s disease in October of 2019 from the fourth neurologist we’d seen in three years (the final three all in 2019 since, before that, I’d believed the neurologist and neuropsychologist who told me nothing was wrong with him). And so I went with that diagnosis—but although the primary reason I needed a diagnosis was for his application for disability coverage, I still wondered if he had frontotemporal degeneration, behavioral variant. And when we finally got to South Carolina (late November 2020) and had an appointment with a wonderful primary care physician (January 2021), she wondered the same thing. But in reality, she did more than wonder. In what I could only see as God directing us to the right physicians, she knew more than some neurologists we’d seen about FTD. And after a review of our story/Tom’s symptoms and records, she said: “I don’t believe for a moment that he has early-onset Alzheimer’s. This is classic FTD.” I couldn’t help but agree. Looks like a duck, walks like a duck—you know the drill. I won’t bore you with the details of our subsequent visit to a South Carolina neurologist who didn’t seem to know a thing about FTD and questioned whether Tom even had dementia. (Seriously? This again?) However, once I sent him the paperwork from the South Florida neurologist (mentioned here), he did sign off on the papers I needed for Tom’s disability application to move ahead. I submitted our part in April of 2020—and, two long sets of paperwork and three phone calls later (they called me to ask more questions)—he finally received the approval letter in February of 2021, two weeks before his March 23 birthday made him eligible for Social Security anyway at age 65. And yet—of course I’m grateful. The letter acknowledged him as “fully disabled” since Nov. 30, 2018—the final date of his employment at the final church where he served. Somehow, that felt satisfying, since that position ended in a horrible way because of his poor judgment and lack of impulse control. The government letter also promised that we would receive back disability payments effective to that date. And, because it’s the government and those wheels grind ever slowly, it took several months for that check to arrive. Yes, it’s good to have, but no, we aren’t suddenly wealthy. For one thing, he has a fairly small Social Security income. For another, I can only use it for needs directly related to his care and support. So that’s what I do. It’s in a special account, and since he can’t manage his finances, the government (after another application and brief wait) named me his representative payee, which means I receive the money and manage it for him. I use it only for expenses directly related to his care, primarily medical and dental needs so far. For example, he had let his teeth go terribly in the years prior to diagnosis, and once the government check came, we could now afford the work he needed to get his mouth back into shape. How all this impacts diagnosis is yet another story. But since (again, if you’re a regular...
read moreSnapshots of Dementia: Love, Actually
Tom and Marti, August 6, 1983 One of my favorite dementia care experts (from whom I’ve learned a lot in the past year) has a particular saying for and about those living with dementia: “I am who I was, but I’m different.” I shared this thought with a dear friend last night as I tried to explain the changes in Tom: He’s still who he was, but he’s different. And on this Valentine’s Day evening, as I sit typing away while my beloved naps on the couch, I realize the concept also holds true about loving someone living with dementia. Back in the day (we met in 1980 and married in 1983), love meant praying together morning and night. Taking time for dates. Sitting on the same side of the table at a restaurant. Kissing after we prayed before meals. Choosing that oh-so-right greeting card. Special gifts (not too often or too extravagant, but always heartfelt.) Making big decisions only as a partnership. Discussing our faith and our children and our lives. And of course, so much more.Today, love looks much simpler. We still pray together at morning and night, but sometimes his thoughts fail to connect. We still have dates, but I plan them all. We still sit on the same side of the table at a restaurant, but only if I remind him. And we still kiss after we pray before meals—but he’s starting to forget that sometimes too. I don’t receive greeting cards or gifts from him anymore unless one of our children helps him find them. I make all the decisions, big and small, and usually don’t mention them to him. He either won’t understand, won’t remember, or both. We still discuss lots of things, but the conversations are much shorter and, of necessity, simpler. Scripture says, “When I became a man, I gave up childish ways” (1 Cor. 13:11b, ESV). Yet Tom is in a stage where he’s embracing childish ways more and more. While I’m working, he’s playing games on his iPad, watching TV, or reading books (he still enjoys reading, although he loses interest easily and can rarely describe the plot). When I’m not working, he still does those things unless I force some sort of needed change. He loves routine, and moving him out of it can upset him.His tastes in food have also gone back to the basic things he loved as a child: carbs. Sweets. Fast food (please don’t send me notes about nutrition; his doctors have agreed that in his situation, comfort food is just that: a comfort. And I do give him a basic healthy diet.) Whether I take him for a simple outing like a visit to Wendy’s or spend time with him watching one of his favorite shows, he will often tell me it’s “the best day ever.” I agree, smiling. I have a lot of those days now—smiling on the outside, heart breaking on the inside. Because the man I have loved and built a life with for so many years is fading away in front of me: repeating his favorite stories to anyone who will listen, forgetting to turn off almost every light he turns on or close almost any door he’s opened. Yes, his short-term memory is that short. And no, none...
read moreSnapshots of Dementia: And Now, the Moment We’ve All Been Waiting For
Photo by Jack Sharp on Unsplash It took us forever to reach this point in mid-September of 2019. In fact, it took not only the visits over three years to neurologists Nos. 1, 2 and 3, but also a 50-plus page questionnaire/application, prayer and what the brain clinic in South Florida said would be a long wait. But only a few days after I submitted the paperwork via certified mail, the clinic called with a sudden cancellation. Could we come in just a few days? You know my answer. As I drove the three-plus hours from Orlando, I prayed this would be that long-awaited moment: The diagnosis that said yes, Tom has dementia. The diagnosis that said yes, it’s FTD (frontotemporal degeneration). The diagnosis that would move him closer to qualifying for disability payments. I decided to travel the distance to neurologist No. 4 because we had reached a stalemate. After two tries, our insurance wouldn’t approve the PET scan neurologist No. 3 said she needed to differentiate between FTD and early-onset Alzheimer’s disease. Already struggling to cover our bills without Tom’s income, I wasn’t about to pay the estimated $5,000 cash for the scan. So I decided to visit one more neurologist—this time, one recommended by the Association for Frontotemporal Degeneration. I hadn’t known to check their list earlier because, until neurologist No. 3, I hadn’t known about FTD. After a slight GPS-induced detour, we arrived for our longest neurology visit to date. I found the team: — Thorough: The group, which included a dietician, physical therapist, nurse practitioner and social worker, met with Tom and me individually and collectively. The exam included neuropsychological testing as well. — Knowledgeable: I knew more about FTD now than I ever had, but this team knew more. That might seem obvious, but it had not proven true with doctors prior to neurologist No. 3. —Caring: This was the first appointment where anyone expressed concern for my mental and emotional health. Just having someone express empathy for our journey meant a lot. The team members were more empathetic than the doctor, who seemed distant, even rude, but I happily accepted knowledge over hand-patting, especially when receiving the latter from anyone came as a surprise. After all the exams and discussions, the entire team met with both of us to give us what they’d promised at the start of our appointment: A diagnosis. In brief, here’s what they said: 1. Tom definitely has dementia. He shows marked impairment in several tested areas, in memory but also in logical sequencing and other elements associated with executive function. His 2019 MRI also shows marked shrinkage from the 2017 one, particularly in the frontal area of his brain, another clear dementia indicator. 2. Tom has a balance problem and needs physical therapy. (I’d spoken with previous neurologists about this and been largely ignored.) 3. My “story,” as the neurologist put it, indicates FTD, behavioral variant, which Tom may have. But the overall testing shows he may have either FTD or early-onset Alzheimer’s. This doctor said Alzheimer’s disease is “a quicker path to disability” (which, I later learned, is not necessarily true) so he would diagnose early-onset Alzheimer’s. Once Tom received approval for disability, he or another neurologist could order the PET scan under Medicare. We now...
read moreSnapshots of Dementia: It’s the Little Things
Photo by Danielle Rice on Unsplash Over the past several months of my somewhat irregular “snapshots of dementia” posts, I’ve written about lots of big things. Our painful journey toward diagnosis. Job losses. Wounds to our marriage and our family. Asking Tom to stop driving. And more. But I’ve also noticed that with dementia as with many areas of life, the little things often have just as much impact as the large ones. Consider the following as not a list of my favorite things but rather of the little things that touch my heart as I watch his early-onset dementia, frontotemporal degeneration, steal so much from my husband. — Open Doors: Tom’s short-term memory has become so short that he rarely remembers to close doors or drawers. You may recall that much earlier, we had to put special hinges on our front door to close it automatically because more than once, he left it standing open when he left for work. Now I can trace his path through our home by the doors and drawers he leaves open. Praise God for a refrigerator with an alarm! — Press Pause: Sometimes I find Tom standing in our hallway, a blank look on his face. Although it passes quickly, I know this means he’s started to go somewhere or do something and forgotten what he started out to do. I can hear some of you saying, “But I do that all the time.” Yes, but probably not fifteen or more times a day—and within only a few seconds of starting the activity. — Delayed Departure: My experience as the mother of five has prepared me well for my current stage of life. As a mom, I had to plan to leave 10 or 15 minutes earlier than the actual departure time because someone wouldn’t have their shoes on or another would need to make a bathroom stop. Even if I tell Tom, “We have to leave in a few minutes,” his broken brain can’t translate that to the steps he must take to be ready to go. In fact, if I give him only two things to do, he will usually forget one of them. These days, we exit more slowly and often have to make a trip or two back inside before our true departure. — “You’re So Smart”: Tom often makes this comment multiple times a day. “You’re so smart” because I could log onto the library website. “You’re so smart” because I knew how to install an app on my phone. “You’re so smart” because I remembered what I had planned for the weekend. What touches my heart here? He never used to say, “You’re so smart” because these were all things he could do for himself. — As a Child: So many things Tom does have become more childlike; in fact, he sometimes talks in a childlike tone. He still enjoys TV and movies, but some of the shows he loves best are the ones he watched as a child. He plays Candyland and other board games with our teenage foster grandson, often losing without realizing why. But simple things seem to thrill him just as they do a child. He often tells me it’s his “best day ever” because we got him two of his favorite...
read moreSnapshots of Dementia: Desperately Seeking Diagnosis
Photo by Raman Oza from Pixabay In a previous episode of “As the Journey Toward Diagnosis Turns,” Tom’s most recent neurologist (No. 3, in case you’re counting) had requested two things to help her solidify Tom’s diagnosis: a PET scan of his brain and the records from the neuropsychologist. Insurance denied the PET scan, but the doctor wanted us to come in anyway. I fought the early-morning Orlando traffic only to discover that the neuropsychologist hadn’t accepted this most recent neurologist’s form, so he hadn’t sent the records. Instead, we had to fill out an additional request. As soon as we completed and signed it, our neurologist’s office faxed it back, believing Tom’s records would arrive soon. We waited. And waited. And ended up having to reschedule because the records still hadn’t arrived. In fact, the neuropsychologist’s office had stopped answering the phone when our neurologist’s office called. Throughout this season of my life, I have had some amazing and supportive medical personnel who have assisted us. But I have also experienced the frustration of dealing with a system that somehow works against rather than for the patient. Why should our health records not be our health records? Why should we have such a difficult time obtaining them to share with another health professional? Fast forward to a few weeks later, another denial of the PET scan by our insurance and another visit to the neurologist. This time, she had the results of the neuropsychological exam. I wasn’t convinced they would help her much, since that practitioner had told us Tom’s only issues were ADHD and shame associated with some of his poor choices. But of course, we were glad to have another appointment. This time, they did another preliminary memory test, and Tom again charmed the nurse’s assistant. I couldn’t tell if he remembered our previous visit or not, but after a brief physical exam and a few more questions, the neurologist explained her dilemma. After reviewing his records, she felt even more confident that he had frontotemporal degeneration, behavioral variant (and by now, I’d done enough reading to agree with her). But she hesitated to make a firm diagnosis without “proof” via a PET scan (I’ve since learned from other FTD spouses as well as medical reports that PET scans do not always provide such proof.) Since our insurance wouldn’t pay for it, we could either wait until Tom turned 65 and get it via Medicare (at that time, nearly two years away), pay for it ourselves (at approximately $5,000) or remain undiagnosed. It may not surprise you that, with my newfound advocacy for my husband, I chose the fourth door: Another neurologist. By this time, I had become connected with the Association for Frontotemporal Degeneration, so I looked at the AFTD website and found just two brain clinics in Florida that they recommended. The first wouldn’t take Tom as a patient. The second would, and although it was more than three hours away and I would have to pay out of pocket, I knew a diagnosis would make it well worth the trip. Besides, if this neurologist was an expert in FTD, surely we would have an answer one way or another. Of course I didn’t expect such an answer at the first visit, but I...
read moreSnapshots of Dementia: Sometimes, We Cry
Unsplash/K. Mitch Hodge I heard Tom before I saw him. As he came through the front door, he sobbed. Working to sort, discard and pack our belongings in advance of putting our Florida home on the market, I’d had a few moments to myself while Tom went with one of our daughters to the county dump. He had driven one car and she, another. (Only a few weeks later, we had to take away his keys.) “Baby! What’s the matter?” I called out as I hurried to meet him. His shoulder shook and the tears poured down his face. “I just hate it when I get things mixed up,” he said. “I bet [our daughter] is so mad at me.” He’d forgotten where the dump was, a lapse that cost them extra time. And no, our daughter wasn’t upset, but it took him several moments to calm down. If you asked Tom about his illness today, he would say he has early-onset dementia, although he might not be able to tell you its name. But back then, we still had no diagnosis, and most of the time, he exhibited the typical FTD anosognosia or lack of awareness of his cognitive lapses and their effects. As our life continued to spiral in scary directions, this proved at best frustrating and at worst maddening. That day, I realized something: I prefer it when he remains unaware. If he doesn’t know he’s forgotten, doesn’t realize he’s caused some sort of problem, doesn’t understand it’s not the website’s fault or the phone’s fault or the television’s fault but his own, he doesn’t understand his decline. And he doesn’t cry. That wasn’t the first day Tom cried, but it was the last for a while. He didn’t cry when, that same week, he made an inappropriate (not sexual) comment to a female friend. He didn’t cry when I put the house on the market. He didn’t cry when, night after night, I would come home from a long day at work, cook dinner, pack or do freelance work while he played on his phone, watched television or slept. He didn’t cry when our children traveled hundreds, even thousands of miles to help us move—or when they left (two for what we thought at the time would be years overseas). The disease has affected the part of his brain that controls emotional reactions, and the damage is uneven. Sometimes his responses are exaggerated, and at other times, blunted. With his and other dementias, what you see happening is not always what you get by way of response. Sometimes, he still cries. We have recently begun attending in-person worship despite his vulnerability to COVID-19 because our church opened up a masks-required section. But every week, he’s cried on the way to church and through part of the service. Although he can’t often articulate his thoughts, I believe he grieves what should still be and, because of his dementia, is not. A job as a pastor. A leadership role. The opportunity to make a real difference in others’ lives. The moments of clarity are often the moments that bring tears. One evening this summer, he seemed especially aware, and I tried to ask how he was feeling about all the changes in our lives. Most of his...
read moreSnapshots of Dementia: More Puzzle Pieces
Photo by Fabiran Kühne on Unsplash Clearly life has gotten in the way of blog posts, and that will happen sometimes. But as I return to the blog, I want to dive back into our journey toward diagnosis (I’m really not trying to make it take as long as the actual journey!). You can find the most recent segment related to diagnosis at this link. In that previous post, I discussed a visit with the third neurologist we saw in our effort to discover what was going on with Tom’s health/memory/behavior and other problems. By this time, I had made some big decisions, most especially the ones that involved selling our home and moving to be closer to family in the upstate of South Carolina (here, we’re closer to our two oldest daughters, one a few minutes away from us and one in Atlanta, only two hours away). I knew that no matter what the doctors said, something was definitely wrong with Tom. I knew he had lost three jobs in quick succession and that we could no longer allow him to drive. And I knew I couldn’t count on him to lead and provide for our family in the way he had for so long. But I still needed help to get a diagnosis. I hoped it would be a path toward disability benefits if, as we thought, he could no longer hold down a job. And I especially needed a diagnosis because I hoped doctors could stop or slow down the disease. This third neurologist was the first one to mention FTD, or frontotemporal degeneration. I’m a writer and editor by profession and also by identity. That means I’m the type of person who will research and read everything I can on any given topic. I’ve already told you more in these posts about FTD than I knew at that point, now about a year and a half ago. But here are some of the key characteristics that stood out to me in my very early research on the topic: —FTD typically strikes younger people (the age range for onset is 21-80, but the majority of cases occur between 45 and 64.) Tom had just turned 63, and I’d suspected problems since well before he turned 60. —FTD is frequently misdiagnosed. Enough said. —FTD is less common and less known than Alzheimer’s. —FTD has no known treatment or cure. This site says, “no current treatments stop or slow the progression of the disease.” And that’s one of the reasons I want to keep writing. As we raise awareness, we can also advocate for research (it’s happening, but slowly) and work toward a brighter future for others faced with this deadly diagnosis. I also learned that FTD has some subtypes including corticobasal syndrome, which affects movement; primary progressive aphasia (PPA), which results in the gradual loss of the ability to speak, read, write and understand speech; and the behavioral variant, which is the type we believe Tom has. There can also be a genetic connection between FTD and amyotrophic lateral sclerois (ALS). Each type is distinct, but as the disease progresses, the symptoms tend to merge. And yes, I do see this merging happening with Tom. Reading about the behavioral variant type was shocking and, in a strange...
read moreSnapshots of Dementia: 7 Facts I Wish I’d Known (Before I Learned by Living)
Pixabay/Gordon Johnson Much of what I’ve shared in these snapshots of dementia so far has a connection to my own ignorance. Of course, you don’t know what you don’t know. So while I don’t blame myself for what I didn’t understand, I sometimes wish I could have a do-over—for Tom’s sake and for my own as well as our family and friends. If a do-over were somehow possible, here are a few of the things I wish I’d known earlier on. 1. Dementia is not a natural consequence of aging. Because one of my grandfathers showed signs of dementia in his 80s and people said, “That’s what happens when you get old,” I honestly thought his age was the primary factor (even though nothing like this happened to my other grandparents, who all lived into their 80s or 90s). I wish I had known more about Grandpa’s problem and even tried to help him more. I think what I saw in him contributed to my misperception (which, I have learned, is common). 2. Dementia is not one but many diseases. Like most people, I’d heard of Alzheimer’s. I knew a little about Parkinson’s Disease, which has related dementia. But I certainly didn’t know about the wide range of dementia disorders, symptoms and problems that exist. Some of the most common in addition to Alzheimer’s include Lewy Body Dementia, vascular dementia and the type my husband has: frontotemporal degeneration or FTD. 3. All dementias are not created equal. This is a corollary to No. 2, because each disease has its own characteristics and qualities. Because Tom’s dementia is still classified as rare (rare enough that many neurologists and other medical professionals seem to have little knowledge of it), I write partly to inform others. I had no idea, for example, that dementia could cause drastic shifts in behavior, personality and ability even at a fairly young age (many FTD patients are much younger than Tom, who, I now believe has shown symptoms for some time). I didn’t know, and as you may have read in the blog, neither did most of our doctors, apparently. 4. Dementia involves more than just memory loss. As explained above, dementias vary from type to type. They can also vary significantly from person to person. Pre-diagnosis, my main perception of dementia was that people who had it grew older, forgot things and became confused. I did not, however, realize that dementia symptoms could include things like loss of the sense of smell (no, this is not the COVID-19 temporary loss); a slowing down in overall thinking; obsessive-compulsive behavior; swallowing issues; apathy and withdrawal from social relationships; language loss and so much more (these are all symptoms Tom has, but they are not the only or even his only symptoms). Some patients don’t show memory loss until they are quite far along into their disease. So why is that the major symptom we associate with dementia? 5. Dementia is a terminal disease. I remember how shocked I was the day I read that FTD will one day kill my husband. Of course, like anyone else, he could die from a number of other causes. But I never understood that the normal course of dementia means that the brain will continue to lose function, which will result...
read moreSnapshots of Dementia: A Merry Heart
Forgetful Jones (Facebook/Sesame Street) “A merry heart does good, like medicine, But a broken spirit dries up the bones” (Prov. 17:22, NKJV). We all have different ideas about dementia; I know I did before we began this journey. And truly, even as transparent as I try to be on my blog, I haven’t yet caught up to present-day except for some occasional glimpses. So this is that! Anyone who knows Tom, in past or present, knows about his trademark sense of humor. Although he has the typical anosognosia (“without knowledge of disease”) of many people with dementia and doesn’t realize the extent of his deficits, he does now know he has frontotemporal degeneration (FTD), and he does know his thinking has changed. He still jokes, although he’s often using lines he’s said for many years. But sometimes his comebacks surprise me, especially since his thinking seems to have slowed down a great deal in the past few months. Last spring, while we still lived in Florida, I made a casual joke about something he would “probably forget.” He looked at me very seriously and said, “I think this is something that is OK for me to joke about, but not OK for you.” Though this may seem like a double standard, I understand exactly what he meant. Many of us women are sensitive about our weight. It might be fine for us to joke about our own chubby tummy or thigh rolls, but we don’t prefer that anyone else do so. And it’s the same with dementia. I’ve been careful ever since to make sure Tom initiates the jokes and/or I only repeat things we’ve said multiple times. As a person created in the image of God, he is and will always be worthy of both respect and love. That being said, Tom has retained his sense of humor. I think I mentioned our joke about his “good ideas” once before. Somehow it has stayed with him that his ideas aren’t the best (to read more about this, see this post.) And so occasionally he will say to me, “I have a great idea!” knowing it may not be, or describe something silly that happens (like this week, when he failed to put the carafe under the coffeemaker and sent coffee all over the counter, then put the top back on incorrectly so that even more coffee spilled) as a “great idea.” I am thankful that having the privilege to work from home has prevented most of the other sorts of “great ideas” from happening. Something else he jokes about is taking his medicine. His short-term memory has become so very short that almost every day, I remind him multiple times to take his medicine (vitamins as well as prescriptions) both morning and evening. He may respond that yes, he will take it, but that doesn’t necessarily mean he will without more reminders. And he may say yes, he has taken it, but that doesn’t necessarily mean he has. So on the days he occasionally misses or doesn’t take his morning dose till late morning, he tells me, “See how much money I’m saving us?” On this, he’s only half-kidding. Always careful with money (except when he was giving it away to online scammers), he is somewhat obsessed with...
read moreSnapshots of Dementia: 3 Lessons From Lincoln for Grandma (and any Caregiver)
Tom meets his grandson, 1 month old. Dear Lincoln, You’re too young to read this although I’m sure, as advanced as you already are, it won’t be long before you are reading not only letters but entire books. First of all, I want to wish you a great big HAPPY BIRTHDAY! Grandpa and Grandma love you very much and can’t believe you’re already 3 years old. As soon as you’re old enough (and hopefully no sooner), someone will tell you about the sad things that happened many years ago on this day. I want you to know that your birthday has given 9/11 new meaning for our family. We do remember the sad things, of course, but we also celebrate the wonderful ones—like you. And do you know what? That’s just who you are in our lives. Your joy in the world God has given us has helped change what might otherwise be a sad time into one of wonder and delight. Watching you play and laugh with Grandpa blesses me more than you can possibly know. You love him in a pure and powerful way that amazes, inspires and challenges me every time. He even told me once that he doesn’t have to worry about what he might say or do around you because he knows you love him no matter what. That is a huge gift to us both. I want to share with you three things I have learned from you, Lincoln. And all three of them help me do a better job taking care of Grandpa. 1. COMPASSION: Grandpa coughs a lot, and sometimes he stumbles. And almost every time you’re around when he does one of these things, I hear you say, “You OK, Gwampa?” Your heart of concern helps me not taking even the smallest or most-repeated issues for granted. Lincoln, Grandpa is always more OK whenever he is with you. 2. PRESENCE: You love nothing more than having Grandpa and Grandma come up to your room and play, or sit beside you on the couch or even travel with you on the iPad as you videochat with us. We love the pictures you color, the cards you “sign” and the crafts you make. But even at only three years old, you’ve already taught me: Presence is the very best present of all. 3. CELEBRATION: Grandpa and I still laugh about the day you told us, “I’m so amazing!” I’m glad you have so much wisdom at such a young age. You are amazing, Lincoln, because of an amazing God who loves you even more than we do and made you “in an amazing and wonderful way” (Ps. 139:14a, NCV). We need to celebrate this on your birthday—and every other day as well. I know you are starting to learn about Jesus. A long time ago, some of Jesus’ followers asked Him who was the greatest. (Even way back then, people worried about silly things like that.) Instead of pointing out the strongest or the biggest or the smartest one, Jesus called over a little child and had everyone look. He told His followers, “I tell you the truth, you must change and become like little children. Otherwise, you will never enter the kingdom of heaven. The greatest person in the kingdom of...
read moreSnapshots of Dementia: Driven to Distraction, Part 1
Photo by Marc-Olivier Jodoin on Unsplash Before we could return to neurologist No. 3 for the second time, a crisis occurred that forced our family into a huge decision. At this point, Tom was still driving. In fact, he was driving for a ride-share company. Sounds crazy for someone who might have dementia, right? Well, yes. And no. Think about it. He had lost three jobs in quick succession. Where could he find work? He loved to drive. And although he struggled with directions now, God and GPS cover a multitude of sins. Add that to the fact that no doctor had diagnosed any specific problem beyond depression, and you’ll see why (although I did have concerns) Tom remained on the road. I discussed Tom’s driving with my adult children (for a while, I had noticed him following more closely than he should) and they agreed that removing driving privileges would be difficult. When necessary, maybe a doctor could make that decision, but not right now. That was our plan. So yes, I’ll go ahead and say it: We were wrong. And I apologize to anyone I may have unknowingly scared or hurt because we were not more proactive. And I pray—and fear—for all of those who may be endangered by those still in the diagnosis or pre-diagnosis process with a disease like Tom’s. I’m convinced; there are many still on the road who should not be. Here’s what happened. Tom was driving for the rideshare company and quite happy to do so. I wasn’t as happy, because he was staying out for longer and longer periods of time. He had a certain daily financial goal, and he would stay out until he reached it. No. Matter. What. Of course, I didn’t know then about the obsessions his type of dementia (frontotemporal degeneration, or FTD) causes (read more about that in this post.) His desire to work and the low pay rate played right into this. The more he drove, the more he wanted to drive. And although I didn’t realize it at the time, I now know he didn’t have the logic or understanding to think, I’m tired. I should stop driving. I need to go home. For him, it truly was all about the money. He was so happy to contribute to our family finances again that he would drive. And drive. And sleep at the side of the road. And drive. As days and weeks passed, I became more and more concerned about his hours. I had more than one serious talk with him where he would promise to “only” work eight hours. Of course, he never kept those promises. At the time, I thought he didn’t want to keep them. Here’s what I didn’t understand: He couldn’t. Within a very short period of time, 10 days or so, several things happened that spurred us to action. The first: Tom got a ticket, not for speeding, but for turning left on red. With a passenger in his car. And with a policeman right behind him. Then and now, I looked on this as providential. The policeman gave him quite the lecture. Maybe it even stuck for a few hours or days. But at least he didn’t cause an accident. I thought the rideshare company might flag...
read moreSnapshots of Dementia: To the Man in the Red Pickup
Dear Man in the Red Pickup, Photo by Neonbrand on Unsplash I know you were angry yesterday morning as you hurried to work. Maybe you were late, and the older couple walking along your route didn’t help. I too have experienced frustration when a biker or pedestrian slowed my progress. It’s no fun, especially when you need to reach your destination on time. And of course, it didn’t help that this road had no sidewalks. What was this couple doing out there anyway? Because I work in a world of words, I often see information as the answer to everything. Still, I realize you may not be interested in information. But since I remained silent while you screamed and swore at my husband, I thought I’d offer more of the story—albeit a little late. You see, there’s at least one thing you couldn’t have known about him: He has an early-onset dementia called FTD (frontotemporal degeneration) that prevents him from making wise, quick decisions. So when you tried to teach him a lesson by staying firmly in your lane yesterday, and he didn’t move, he wasn’t being stubborn—at least, not in the way you or I might be. He simply isn’t able to process a concept such as “A truck is coming. It may not stop or move over. I should get out of the way” fast enough to do what you expected. I realize you saw his behavior as arrogant and rude. But this is far from the truth. Until about two years ago, he was a pastor who loved (and still loves) God and people. Even at his best, he would have thought you should respect him as a pedestrian, but I doubt he would have challenged you by remaining in your lane. Now, he just can’t think fast enough to move over, even when I tell him to (which I did as you approached us). So even though you told him, “Next time, I won’t stop,” I’m not sure he has the mental ability to change his behavior. My husband’s dementia also causes obsessions. One of his current ones is walking, and so the two of us walk at least 3.5 miles every morning and nearly that far every evening when he’s not too tired (his dementia also causes exhaustion). Several months ago, our family made the decision not to let him walk alone anymore. Although he knows about the COVID-19 pandemic and social distancing, he can’t follow the steps needed to carry out those restrictions on his own. His lack of logic also means that more than once, I’ve had to pull him back from crossing a street as a car headed right toward him. Why do we walk on that road where you met us? As you know, few streets in our area have sidewalks, and that route happens to be my husband’s favorite. We go early in the morning (we leave at 6:30 or 6:45 a.m.) when traffic is light. Yes, we could walk at the local rec center, but until now, I’ve felt safe on the roads. I had already told him that when school started back, we might have to readjust our route. He has lost so many freedoms (he cannot work or drive anymore) that I didn’t want to take...
read moreSnapshots of Dementia: The Great Depression (or not)
Photo by Stefano Pollio on Unsplash If your snapshots are anything like mine, they fill a shoebox (OK, mine fill an entire trunk) and most are in random order. I have long-ago dreams of putting them in beautiful, chronological albums (I’m sure God has a special place in heaven for those who have achieved this wondrous feat), but so far, it hasn’t happened. I don’t think it will happen with these snapshots either. So, although I’ve written somewhat chronologically, you may have noticed I’ve also skipped back, forth and around as I’ve focused my lens on different parts of our journey and of Tom’s disease. And I imagine that, even if you’ve never been exposed to dementia before, you’ve seen that this disease is exactly like that. Messy. Disorganized. Uncomfortable. I’ll move us forward a bit on our timeline to our visits with a second neurologist. We’re all the way up to early 2019 now, and many things have changed for Tom. Just the year before, his first neurologist told us (for the second time) that things were basically fine, that he just had some short-term memory loss and (for the first and only time) that he was “better than the 80-year-old Alzheimer’s patients I see.” A neuropsychologist had also done extensive testing (which I eventually found out our insurance did not cover, although no one told me that at the time; I mention this so anyone reading will check first and not have to shell out the nearly $1800 I did almost a year later). This doctor concluded that Tom was very intelligent, probably had adult ADHD (a diagnosis he had already received) and was dealing with shame as the result of some of his extremely poor and uncharacteristic behavioral choices over the past few years. No one told us about frontotemporal degeneration (FTD), behavioral type. No one mentioned that dementia could not only cause memory loss and confused thinking but that it could also cause personality changes of the extreme type we saw in Tom. No one mentioned that perhaps he didn’t have a moral problem but a mental one. That’s why I have such a deep commitment to tell our story. I did suspect a problem; I just didn’t realize so much of what I was seeing in my husband was tied to what we now know to be FTD. But I digress. Finally, we visited a second neurologist. This one came recommended from more than one friend. I was confident that this time, we would get some answers. So much had changed in Tom’s life that I felt sure the doctor would see the problems right away. We had (well, I had, because Tom could no longer fill out anything so complicated) lots of paperwork to fill out before this visit, but I didn’t mind. I wanted the doctor to have information. I even added a copy of a letter from our former pastor about the changes he had seen in Tom’s work ability, moving from “highly competent” to much less than that over the more than five-year period Tom had served under him. At this visit, the neurologist and her staff asked lots of questions. In fact, we spoke more with the staff than we did with the doctor. She examined Tom briefly and...
read moreSnapshots of Dementia: The Best Present of All
Andrew and Tom, Christmas Eve, 2023 From our wedding day forward, music has been an essential part of our family life. Tom wrote our wedding processional. We had a playlist for my labor with our children long before it was popular to have one. As a family, we’ve collectively memorized thousands of lyrics to children’s and adult musicals, often while riding together in the car. And although none of our children is a professional musician as their dad was, they all love music. The title for this post, in fact, comes from a song I remember them listening to many years ago (Donut Man, anyone?). We are celebrating double Christmases this year. The first took place on December 25 with my mother (pickup and return to and from Ohio courtesy of our two oldest daughters) and nearby family members. The second will take place next weekend, when all our children except our daughter and son-in-love from Texas will join us for another family celebration. We haven’t yet exchanged gifts with our children; that will happen during the second Christmas. Still, some gifts have already arrived. Even as late as last year, Tom would sometimes tell people he was a professional trumpet player. The truth is, he has barely touched his horn since May of 2016, when he injured his lip during a challenging concert of the Florida Worship Choir & Orchestra (Tom is one of two first trumpet players in the linked video of one song from this concert). I wrote here about how what I now know was emerging dementia kept him from a full recovery, effectively ending his trumpet career. Although he used to play simple songs for our grandson, he has not done that for more than a year, and he rarely touches his trumpet. This may not seem unusual, but his practice was so consistent for so long that my children and I can all sing the notes of his Stamps-Baxter warmup. While working as a pastor and worship pastor, he continued to perform and to teach trumpet, instructing hundreds of trumpet students over the years. He had only one failed student: our son. After several months of working together, he and Andrew agreed to part musical ways, and Andrew went on to other areas of interest. That was true until dementia happened to Tom and then the pandemic happened to the world. During that terrible season, God gave Andrew the idea to help reawaken his Dad’s interest in trumpet. He bought a horn and, via YouTube, restarted his trumpet instruction. As he improved, he started connecting with his Dad via Zoom, and they used that platform to practice simple duets. But Andrew’s efforts failed to increase Tom’s interest in his former passion. He would play his horn when our son took the initiative, either by Zoom or in person, but unless Andrew reached out, no practice would occur. If I reminded Tom, he might or might not get his horn out—and even if he did, he would play for no more than a few minutes. Gradually, I gave up the hope that he could return to playing. Over the past few months, our family and friends have watched Tom take a steeper nose dive. Simple questions or instructions confuse him. He still sings with the choir...
read moreSnapshots of Dementia: At Just the Right Time
Tom uses his trumpet to draw people to the area where our mission team would present a gospel-based drama, San Jose, Costa Rica, 2014. A few years ago, I lived a much different life in a different place than the one I have right now. Living near Orlando, Florida, where Tom served as a worship pastor, I worked as a freelance writer and editor as I do now, but since Tom was the primary breadwinner, it didn’t matter that my income went up and down with the assignments. As my children grew, I traveled, often to teach at Christian writers conferences across the United States. But the travel I enjoyed most was a luxury I no longer have: going overseas to serve in missions and write the story of those trips, either in online blog format or in print. I consider any assignment that combines my love for young people, prayer, missions, and writing a huge win, and these trips, designed to give students a short-term missions experience, provided all of that. Once, I brought Tom along on a trip to Costa Rica; he had led international mission trips with the various churches we had served, but we had never gone together before—a bonus blessing. Another time, I had the opportunity to serve alongside our youngest daughter in Panama for the final ten days of her five-week trip, another bonus blessing. At least for right now, the international travel is no more. The up-and-down income is no more. But the blessings of those trips continue, largely in the form of relationships. Thanks to those trips, I have friends across the U.S., Canada, and Latin America (where all of my mission trips took place). And those friends—many of whom were high school or college students when we met—continue to encourage me today. What does this have to do with dementia? A lot. Not only has Tom’s life changed with the onset of his disease, but mine has too—in the ways listed above and more. I tend to live on the side of hope and not discouragement. But as his disease progresses, I do have moments, even seasons, of concern. Not long ago, my mother had some health struggles at the same time as I saw some sudden declines in Tom. I found myself in need of extra rest, and at first I couldn’t figure out why. But before long, I realized: The internal stress was wearing me down. I didn’t find an immediate fix for my situation, but the habits I already have in place kept the issues from escalating. God also provided help in ways I had not expected: Understanding words from family members. A special opportunity to reach beyond my problems by serving my church family in a new way. And—without my mentioning any of my concerns—texts and messages from some of the same students I’d served alongside on the mission field, all of which arrived on God’s schedule: at just the right time. One of these unexpected messages came from a young woman I remembered from mission trips. I woke up to early writing assignments that day and happened to see her note waiting for me. Tears came to my eyes as I read her words of encouragement. This was a person with whom I’d had little contact since those...
read more